Accelerating Science to Improve Early Autism Screening
• Feature Story • 75th Anniversary
At a Glance
- Autism is a neurodevelopmental disorder that affects how people interact, communicate, and learn.
- Making early autism screening part of routine health care helps connect families to support and services as early as possible.
- Despite American Academy of Pediatrics guidelines, only a small fraction of pediatricians reported screening for autism at well-child visits.
- NIMH-supported efforts to close the gap between science and practice have yielded key insights into effective strategies for expanding early autism screening.
- Researchers are identifying new tools for detection, new models for delivering services, and new strategies for embedding early autism screening and rapid referral into routine health care.
As many parents of young children know all too well, visits to the pediatrician typically involve answering a series of questions. Health care providers may ask about the child’s eating and sleeping habits or about their progress toward walking, talking, and many other developmental milestones. Increasingly, they’re also asking questions that could help identify early signs of autism.
Autism is a neurodevelopmental disorder that affects how people interact, communicate, behave, and learn. It is known as a “spectrum” disorder because there is wide variation in the type and severity of symptoms people experience.
Today, thanks to research focused on embedding routine screening in well-baby checkups, the early signs of autism can be identified in children as young as 12–14 months. These efforts, many supported by the National Institute of Mental Health (NIMH), show that making early autism screening part of routine health care can have a significant impact on children and families, helping connect them to support and services as early as possible.
“This progress wasn’t inevitable or linear,” explains Lisa Gilotty, Ph.D., Chief of the Research Program on Autism Spectrum Disorders in the Division of Translational Research at NIMH. “Rather, it’s part of an evolving story that reflects the persistent, collective efforts of researchers and clinicians working to translate science into practice.”
Identifying the disconnect
The modern concept of autism as a neurodevelopmental disorder first emerged in the 1940s and coalesced into a diagnostic label by the 1980s. Diagnostic criteria evolved over time and, by the early 2000s, clinicians had evidence-based tools they could use to identify children with autism as early as 36 months. At the same time, evidence suggested that parents may notice signs even earlier, in the child’s second year of life.
“Reducing this gap—between observable signs and later identification and diagnosis—became an urgent target for researchers in the field,” said Dr. Gilotty. “The research clearly showed that kids who were identified early also had earlier access to supports and services, leading to better health and well-being over the long term.”
Researcher Diana Robins, Ph.D. , then a doctoral student, wondered whether an evidence-based early screening tool might help close the gap. With support from NIMH , Robins and colleagues developed the Modified Autism Checklist for Toddlers (M-CHAT) , which they introduced in 2001. They aimed to provide pediatricians with a simple screening measure that could identify children showing signs of autism as early as 24 months.
The science behind early screening continued to build and gain momentum over the next few years. By the mid-2000s, researchers were exploring the possibility of using various developmental screening tools—such as the Communication and Symbolic Behavior Scales, First Year Inventory, and Ages & Stages Questionnaires—to identify early signs of autism.

The growing body of evidence did not go unnoticed. In 2006, the American Academy of Pediatrics (AAP) issued evidence-based guidelines recommending autism-specific screening for all children at the 18-month visit. In a later update, they recommended adding another autism-specific screening at the 24-month visit, recognizing that some children may start showing signs a bit later in development.
To the research community, these new guidelines signified a huge step forward for science-based practice. But this sense of progress was soon dashed by reality.
When researchers actually surveyed health care providers, they found that very few knew about or followed the AAP guidelines. For example, in a 2006 study , 82% of pediatricians reported screening for general developmental delays, but only 8% reported screening for autism. Most of the pediatricians said they weren’t familiar with autism-specific screening tools, and many also cited a lack of time as a significant barrier to screening.
The disconnect between science and practice prompted concern in the research community. A series of conversations in scientific meetings and workshops led to a crystallizing moment for the staff at NIMH.
“There was a period of several years in which researchers would go off and do unfunded work and then bring it back to these meetings and say, ‘This is what I've been working on,’” said Dr. Gilotty. “It was an impetus for those of us at NIMH to say, ‘We’re going to do something about this.’”
Bridging the gap
Gilotty worked with colleagues Beverly Pringle, Ph.D., and Denise Juliano-Bult, M.S.W., who were part of NIMH’s Division of Services and Intervention Research (DSIR) at the time, to synthesize several file drawers’ worth of different measures, meeting notes, and research papers and distill them into an NIMH funding announcement.
The announcement, issued in 2013, focused on funding for autism services research in three critical age groups: toddlers , transition-age youth , and adults . NIMH ultimately funded five 5-year research projects that specifically examined screening and services in toddlers. The projects focused on interventions that emphasized early screening and connected children to further evaluation and services within the first two years of life.
In 2014, Denise Pintello, Ph.D., M.S.W., assumed the role of Chief of the Child and Adolescent Research Program in DSIR. She directed the research portfolio that included these projects, which sparked an idea:
“It was such an exciting opportunity to connect these researchers because the projects were all funded together as a cluster,” she said. “I thought, ‘Let’s encourage these exceptional researchers to work closely together.’”
At NIMH’s invitation, the researchers on the projects united to form the ASD Pediatric, Early Detection, Engagement, and Services (ASD PEDS) Research Network. Although the ASD PEDS researchers were using different research approaches in a range of settings, coming together as a network allowed them to share knowledge and resources, analyze data across research sites, and publish their findings together . The researchers also worked together to identify ways that their data could help address noticeable gaps in the evidence base.
Building on the evidence
Together, the ASD PEDS studies have screened more than 109,000 children, yielding critical insights into the most effective strategies for expanding early autism screening.
For example, an ASD PEDS study led by Karen Pierce, Ph.D. , showed the effectiveness of integrating screening, evaluation, and treatment (SET) in an approach called the Get SET Early model.
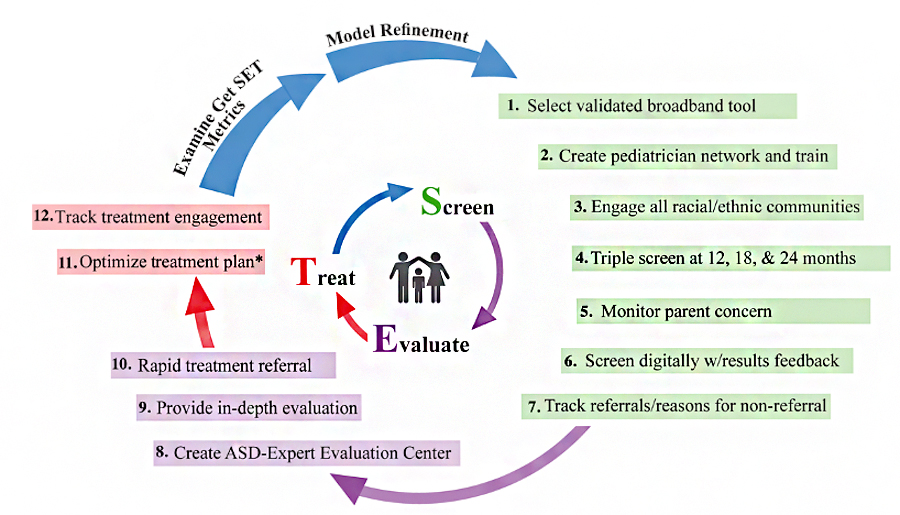
Working with 203 pediatricians in San Diego County, California, Pierce and colleagues devised a standardized process that the providers could use to screen toddlers for autism at their 12-, 18-, and 24-month well-child visits. The researchers also developed a digital screening platform that scored the results automatically and gave clear guidelines for deciding when to refer a child for further evaluation.
These improvements boosted the rate at which providers referred children for additional evaluation and sped up the transition from screening to evaluation and services. The study also showed that autism can be identified in children as young as 12–14 months old, several years earlier than the nationwide average of 4 years.
This and other studies showed that incorporating universal early screening for autism into regular health care visits was not only feasible but effective. Working closely with health care providers allowed researchers to build trust with the providers and address their concerns.
“There is this sense that if you sit down and really talk with pediatricians, you can bring them into the fold,” said Dr. Gilotty. “Once you get some key people, you get a few more and a few more, and then it becomes something that ‘everybody’ is doing.”
Meeting the need
At the same time, the ASD PEDS studies have also explored ways to reach families with young children outside of primary care settings. Numerous studies have shown that some families are much less likely to have access to early screening and evaluation, including non-English-speaking families, families with low household incomes, and families from certain racial and ethnic minority groups.
“Screening is most effective when everyone who needs it has access to it,” said Dr. Pintello. “Addressing these disparities is a critical issue in the field and NIMH’s efforts have prioritized focusing on underserved families.”
One way to accomplish this is to integrate standardized universal screening into systems that are already serving these families. For example, in one study, ASD PEDS investigators Alice Carter, Ph.D. , and Radley Christopher Sheldrick, Ph.D. , worked with the Massachusetts Department of Public Health to implement an evidence-based screening procedure at three federally funded early intervention sites.
The researchers developed a multi-part screening and diagnosis process that included both clinicians and caregivers as key decision-makers. They hypothesized that this standardized process would minimize procedural variations across the early intervention sites and help to reduce existing disparities in ASD screening and diagnosis.
The results suggested their hunch was correct. All three study sites showed an increase in the rate of autism diagnosis with the new procedure in place, compared with other intervention sites that served similar communities. Importantly, the standardized procedure seemed to address existing disparities in screening and diagnosis. The increased rate of diagnosis observed among Spanish-speaking families was more than double the increase observed among non-Spanish-speaking families.
Looking to the future
Researchers are continuing to explore the best ways to put existing evidence-based screening methods into practice. At the same time, NIMH is also focused on research that seeks to develop new and improved screening tools. Evidence from neuroimaging and eye tracking studies suggests that, although the age at which observable features of autism emerge does vary, subtle signs can be detected in the first year of life. NIMH is supporting a suite of projects that aim to validate screening tools that can be used to identify signs of autism before a child’s first birthday.
“In other words, are there measures we can use to identify signs even before parents and clinicians begin to notice them?” explained Dr. Gilotty. “This is the critical question because the earlier kids are identified, the earlier they can be connected with support.”
These projects leverage sophisticated digital tools to detect subtle patterns in infant behavior. For example, researchers are using technology to identify patterns in what infants look at, the vocalizations they make, and how they move. They’re using technology to examine synchrony in infant–caregiver interactions. And they’re developing digital screening tools that can be administered via telehealth platforms.
The hope is that new tools identified and validated in this first stage will go on to be tested in large-scale, real-world contexts, reflecting a continuous pipeline of research that goes from science to practice.
“As a result of targeted research funded by NIMH over the last 10 years, we are seeing new tools for detection, new models for delivering services, and new strategies for embedding early screening and rapid referral into routine health care,” said Dr. Pintello.
“I feel like it’s just the beginning of the story—we are just now seeing the impact of bringing science-based tools and practices into the hands of health care providers. Over the next few years, we hope that ongoing efforts to bridge science and practice will help us meet the unique needs of children at the exact time that they need services.”
Publications
Broder Fingert, S., Carter, A., Pierce, K., Stone, W. L., Wetherby, A., Scheldrick, C., Smith, C., Bacon, E., James, S. N., Ibañez, L., & Feinberg, E. (2019). Implementing systems-based innovations to improve access to early screening, diagnosis, and treatment services for children with autism spectrum disorder: An Autism Spectrum Disorder Pediatric, Early Detection, Engagement, and Services network study. Autism,23(3), 653–664. https://doi.org/10.1177/1362361318766238
DosReis, S., Weiner, C., Johnson, L., & Newschaffer, C. (2006). Autism spectrum disorder screening and management practices among general pediatric providers. Journal of Developmental and Behavioral Pediatrics, 27(2), S88–S94. https://doi.org/10.1097/00004703-200604002-00006
Eisenhower, A., Martinez Pedraza, F., Sheldrick, R. C., Frenette, E., Hoch, N., Brunt, S., & Carter, A. S. (2021). Multi-stage screening in early intervention: A critical strategy for improving ASD identification and addressing disparities. Journal of Autism and Developmental Disorders, 51, 868–883. https://doi.org/10.1007/s10803-020-04429-z
Feinberg, E., Augustyn, M., Broder-Fingert, S., Bennett, A., Weitzman, C., Kuhn, J., Hickey, E., Chu, A., Levinson, J., Sandler Eilenberg, J., Silverstein, M., Cabral, H. J., Patts, G., Diaz-Linhart, Y., Fernandez-Pastrana, I., Rosenberg, J., Miller, J. S., Guevara, J. P., Fenick, A. M., & Blum, N. J. (2021). Effect of family navigation on diagnostic ascertainment among children at risk for autism: A randomized clinical trial from DBPNet. JAMA Pediatrics, 175(3), 243–250. https://doi.org/10.1001/jamapediatrics.2020.5218
Pierce, K., Gazestani, V., Bacon, E., Courchesne, E., Cheng, A., Barnes, C. C., Nalabolu, S., Cha, D., Arias, S., Lopez, L., Pham, C., Gaines, K., Gyurjyan, G., Cook-Clark, T., & Karins, K. (2021). Get SET Early to identify and treatment refer autism spectrum disorder at 1 year and discover factors that influence early diagnosis. The Journal of Pediatrics, 236, 179–188. https://doi.org/10.1016/j.jpeds.2021.04.041
Robins, D. L., Fein, D., Barton, M. L., & Green, J. A. (2001). The Modified Checklist for Autism in Toddlers: An initial study investigating the early detection of autism and pervasive developmental disorders. Journal of Autism and Developmental Disorders, 31, 131–144. https://doi.org/10.1023/A:1010738829569
Sheldrick, R. C., Carter, A. S., Eisenhower, A., Mackie, T. I., Cole, M. B., Hoch, N., Brunt, S., & Pedraza, F. M. (2022). Effectiveness of screening in early intervention settings to improve diagnosis of autism and reduce health disparities. JAMA Pediatrics, 176(3), 262–269. https://doi.org/10.1001/jamapediatrics.2021.5380
Learn more
- NIMH Health Information Page: Autism Spectrum Disorder
- NIMH Brochure: Autism Spectrum Disorder
- NIMH Statistics Information: Autism Spectrum Disorder (ASD)
- NLM MedlinePlus: Autism Spectrum Disorder
- HHS Interagency Autism Coordinating Committee