The Ups and Downs of Bipolar Disorder
• Feature Story • 75th Anniversary
This story is part of a special 75th Anniversary series featuring the experiences of people living with mental illnesses. The opinions of the interviewees are their own and do not reflect the opinions of NIMH, NIH, HHS, or the federal government. This content may not be reused without permission. Please see NIMH’s copyright policy for more information.
Note: This feature article contains references to suicide and self-harm, which may be triggering to some. If you or someone you know has a mental illness, is struggling emotionally, or has concerns about their mental health, there are ways to get help. If you are in crisis, call or text 988 to connect with the 988 Suicide & Crisis Lifeline . To learn more about bipolar disorder and ADHD, visit NIMH’s bipolar disorder and ADHD health information pages.

Somewhere between Boston and New Hampshire’s White Mountains, Josh Santana lost touch with reality.
The shift marked a stark divergence for the young college student, as the preceding weeks had ranked among the best he could remember. He no longer needed an alarm clock to wake up. He ran his fastest mile. He walked for hours at night, contemplating how to better the world. But the best part, he said, was as if overnight, years of mental illness vanished. His pain, the depression, the restlessness—all of it—ceased.
“It was such a wave of euphoria that initially I was like, ‘I finally broke out of it. I’m no longer mentally ill,’” Santana said.
The milestone was short-lived. Two weeks later, still euphoric, Santana’s judgment began to decline.
He talked to strangers about the future. He conjured ways to shift the planets. He lost trust in his friends. His strongest advocate, his mother, worried. Then, on a whim, he skipped out on a teaching gig. And somewhere along a dark mountain road, he thought about driving off a bridge.
“By that point, the people around me had seen such a stark difference in my behavior that, when I pulled into my home, I was surrounded by three cop cars,” Santana said. “Somebody had reported that they were worried about me.”
What Santana, then 21, had experienced was a significant episode of mania—a serious and dangerous symptom of bipolar disorder.
“People with bipolar disorder experience periods of ‘highs,’ with mania and euphoria or irritability. These periods alternate with episodes of depression or ‘lows,’ with a loss of interest, motivation, concentration, and energy,” said Matt Rudorfer, M.D., chief of the Adult Psychopharmacology, Somatic, and Integrated Treatment Research Program at the National Institute of Mental Health (NIMH).
But it’s more than just mood swings. The changes can be extreme, and episodes can last from days to months. Further, bipolar disorder is associated with the risk of suicide, Dr. Rudorfer said.
“The life disruptions caused by bipolar disorder are not well-controlled, making it hard to focus, to think clearly, and in extreme cases, to tell what’s real and what is not,” he said. “This can make it difficult or impossible to function at work, school, or home.”
For Santana, the episode was a low point in his life and the culmination of a long history of mental illness.
When life revolves around mental illness
Now 27, and a successful real estate agent and musician, Santana bears no resemblance to the once-manic college student. He’s articulate, organized, and driven to excel.
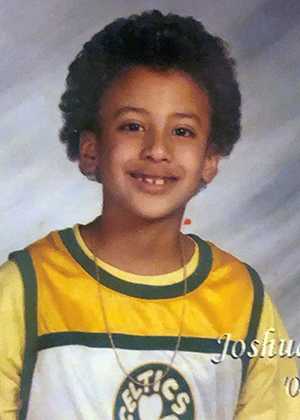
Recently, he was featured in the book, You Are Not Alone, by Ken Duckworth, M.D., Chief Medical Officer of the National Alliance on Mental Illness. Reflecting on the lessons learned from his challenges with mental illness, Santana told Dr. Duckworth his difficulties began at a very young age.
“I got removed from mainstream preschool because I assaulted a teacher during a behavioral outburst,” he told Dr. Duckworth. “I was 4 years old and wasn’t permitted to return to mainstream kindergarten unless my mom agreed to have me psychologically evaluated and have a paraprofessional stay with me throughout my entire kindergarten year as well. From 5 years old and on, I was heavily medicated, and a lot of those initial years were a blur.”
It was a rough start for the young child, and Santana later learned that his difficulties arose from attention-deficit/hyperactivity disorder (ADHD). The disorder is marked by an ongoing pattern of inattention and/or hyperactivity and impulsivity that interferes with functioning or development.
Though academically gifted—learning the basics of algebra at age 8—Santana said he felt ADHD hindered his cognitive development. While his work was excellent, and he aced all the tests, teachers failed him for conduct.
These failures led to feelings of shame and guilt, he said.
“The hardest part was the physical energy management on my end because there were so many situations where I would have to contain myself, and I had to internalize some of that angst,” Santana said. “I think having the behavioral issues and excess energy prevented me from being able to focus and nurture that [gifted] part of me from an earlier age.”
Though he’s never met Santana, Dr. Rudorfer said the pattern of behavioral outbursts is common with ADHD.
“Typically, boys with this disorder will be physically hyperactive, with trouble sitting still, in some cases running around the classroom, leading to frequent trips to the principal’s office,” Dr. Rudorfer said, adding that ADHD can persist into adulthood.
For Santana, ADHD was just the beginning. Bouts of anxiety and depression followed around sixth grade, creating within him layers of mental illness. This led to more medication, until, at one point, he was cycling through a “never-ending menu” of prescriptions. During this time, Santana experienced lulls and “windows of stability,” where a wave of mental illness would subside, only to be replaced by another.
By the time he turned 15, Santana had started experiencing the symptoms of bipolar disorder. His doctor prescribed more medication, this time, antipsychotics.
“My life fully revolved around my mental illness: If I was depressed, I wasn’t doing homework. If I was hyper, I wasn’t doing homework,” Santana said. “Throughout high school, I had a lot of ups and downs because of that. I also had a lot of elevated moods where I would spend a lot of time doing unsafe things.”
My life fizzled away
By college, Santana was able to manage his symptoms, but the array of medications sedated him. He slept 13 hours a day and would fall asleep in class and while driving.
When the psychiatrist he had seen since he was 5 abruptly retired, Santana stopped taking his medication. A manic episode soon followed. While everyone around him could see the changes in his behavior, Santana couldn’t see the changes himself.
“In my head, I was like, ‘Finally, … I’m ready to make a difference,’” he said. “For the most part, it felt good, until the end, right before I went into emergency care.”
The police arriving at his house after the mountain drive sobered Santana to the realization that he wasn’t okay. He entered a form of outpatient care called partial hospitalization.
As the mania faded, reality set in. In those last two weeks, Santana had destroyed relationships, some with longtime friends.
“Sometimes, the emotional symptoms of bipolar do not reflect the intentions underlying the actual person,” he said. “And it’s one of the reasons why the guilt comes so strong afterward, because you’re like, ‘Who the hell was that?’”
Immediately, he fell into another depressive episode.
“I was seeing my whole life fizzle away,” he said.
The road to recovery
During the partial hospitalization, doctors adjusted Santana’s treatment plan, and slowly, he began to stabilize. As he continued with therapy, Santana winnowed his medications down to just two—at low doses. He also found a treatment regimen that worked and stuck with it.
He credits this combined effort—therapy, coping mechanisms, perfecting his routines for eating and sleeping, and mindfulness practice—as playing a significant role in his recovery.
“It was a mix of everything,” he said. “It seems like people’s situations can be so unique, and we often want a quick fix … but it was a lot of trial and error.”
Dr. Rudorfer acknowledged treatment isn’t always easy.
“Finding the right medication—and even the right dose of a specific medication—can be challenging. Everyone is different, and it takes a while to see how the brain will respond to treatment while trying to keep any side effects to a minimum. Many people have other conditions co-existing with bipolar disorder, which compounds these challenges and often requires a combination of medications for best results,” Dr. Rudorfer said.
The important thing is to maintain good communication with your health care provider and to give the medication time to work while following through with all parts of the treatment plan, including therapy and attention to the sleep-wake cycle, Dr. Rudorfer explained.
“While the process can be difficult, people can get better with proper treatment. Today’s therapeutic regimens aim not merely to reduce symptoms—but to achieve life-changing and life-saving true remission and recovery,” he said.
In time, Santana returned to school. He made a concerted effort to make amends for his past behavior and better himself. He adopted a dog, Koda, completed his master’s degree in music, earned his real estate license, and joined a nonprofit orchestra for people with mental illnesses.
Now recovered, Santana’s life no longer revolves around mental illness. He’s healthy, thriving, and happy. It was a long journey, but one he said was worth taking.
“I’m at a point where mental illness hasn’t played such a big role in my life—and it feels good,” he said.
