Novel Treatment Helps Children With Severe Irritability
• Research Highlight
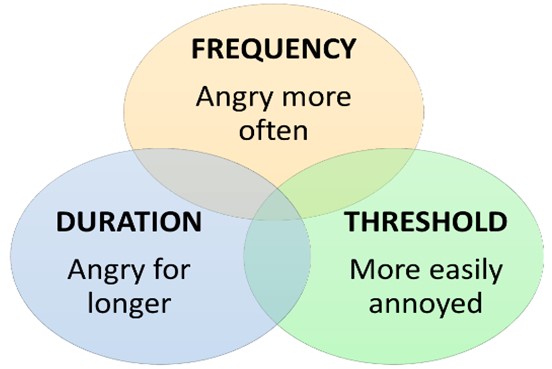
A persistent state of anger or annoyance coupled with frequent and intense temper outbursts in children and adolescents often signals clinically impairing irritability. Clinical irritability disrupts a child's daily life and can continue to cause problems into adulthood. Although irritability is one of the leading reasons children are seen for psychiatric care, it is understudied compared to other childhood disorders. Critically, evidence-based treatments for clinical irritability are also lacking.
In a new study, researchers at the National Institute of Mental Health (NIMH) successfully used exposure-based cognitive behavioral therapy (CBT) to treat severe irritability in children. This promising breakthrough underscores the importance of tailored interventions in this area of child psychiatry.
What is severe irritability in children?
This study focused on severe and impairing irritability and temper outbursts in youth. All children feel angry or irritable at times. Severe irritability is more serious and can cause problems at home, during school, and with friends.
Irritability and outbursts are part of many mental disorders, but they are core symptoms of disruptive mood dysregulation disorder (DMDD). DMDD is diagnosed in children and adolescents who show ongoing irritability, frequent anger, and intense temper outbursts.
Symptoms of DMDD are severe and require treatment. Children with this high level of irritability get angry often and to a degree that is disproportionate to the situation and their age. When angry, they show temper outbursts, usually involving high motor activity and verbal or physical aggression. These children are also persistently irritable or cranky most of the time and across many situations.
How did the researchers treat severe irritability in children?
Researchers led by Melissa Brotman, Ph.D., in the NIMH Intramural Research Program tested a novel treatment for irritability. Developed in Dr. Brotman’s lab, the exposure-based CBT treatment draws on a highly effective treatment for anxiety—exposure therapy. In this pilot study, the researchers examined the effectiveness, acceptability, and feasibility of exposure therapy for severe irritability.
Forty children (8–17 years) participated in the study, which took place at the NIH Clinical Center . Children had to have at least one of two core DMDD symptoms: chronically irritable mood or severe temper outbursts. Some children also had co-occurring anxiety or attention-deficit/hyperactivity disorder (ADHD), but they were not eligible for participation if diagnosed with other disorders, such as bipolar disorder, substance use disorder, schizophrenia, or autism spectrum disorder.
All children received 12 sessions of exposure-based CBT following an established manual written by Dr. Brotman. Each treatment session had a child and a parent portion.
- The child portion focused on increasing tolerance to frustration. Clinicians carefully exposed children to anger-provoking situations, gradually moving up a hierarchy specific to that child. Examples could be taking away a preferred item (for example, stopping a video game or getting off the iPad) or starting a disagreeable activity (for example, brushing teeth or doing homework). Clinicians worked with the child to learn to tolerate and constructively respond to their feelings without a temper outburst.
- The parent portion focused on parent management skills. Parents were taught to actively ignore their child’s temper outbursts to stop reinforcing those behaviors. Instead, they learned how to focus on and consistently reward positive behaviors.
Children were randomly assigned to be observed for either 2, 4, or 6 weeks before starting treatment. Clinical observers were blind to when active treatment began. This observation period allowed the researchers to confirm that symptoms changed only after treatment started and were not accounted for by the clinician’s expectations of the treatment.
Clinicians, children, and their parents rated the child’s irritability symptoms and overall functioning during the observation period, during treatment, and 3 and 6 months after treatment. Depression, anxiety, and ADHD symptoms were also assessed for comparison. The acceptability, feasibility, and safety of the therapy were determined by rates of study dropout and adverse events.
Did exposure-based CBT treatment help children with severe irritability?
Irritability symptoms decreased significantly during treatment based on clinician, child, and parent reports. Overall functioning also improved—by the end of treatment, 65% of children were significantly improved or recovered based on the clinician measure. Symptoms did not return after treatment stopped and, in fact, treatment gains were maintained at the 3- and 6-month follow-ups.
When examining the core symptoms of DMDD, 60% of children were considered recovered on the Temper Outburst scale and 25% were recovered on the Irritable Mood scale at the end of treatment. This result suggests a stronger effect of exposure therapy in decreasing temper outbursts compared to improving irritable mood. In contrast, the treatment was not associated with significant changes in anxiety, depression, or ADHD symptoms, suggesting its specificity in targeting irritability.
No families dropped out once treatment began, suggesting exposure therapy was acceptable and feasible. Similarly, no adverse events were reported, supporting the safety of using exposure therapy with children.
What can researchers do next to further treatment for children with severe irritability?
Taken together, these results support the effectiveness, acceptability, and feasibility of exposure therapy for youth with severe irritability. Irritability symptoms and overall functioning improved during treatment per clinician, child, and parent reports and were maintained for several months after treatment stopped.
This study has some limitations. First, it had a relatively small sample size with a limited racial, ethnic, and socioeconomic composition, which limits the generalizability of the results. Second, the study did not include a control group of children with irritability who did not receive treatment. Although the researchers addressed this concern by having multiple observation periods, comparing this novel treatment to current clinical care is a critical next step. Third, the study included a wide age range, making it important to test whether there are differences in outcomes based on age. Last, because clinicians delivered the child and parent components at the same time, future studies could examine the individual contribution of child exposure therapy versus parent management skills to determine whether one is driving treatment effects.
The positive results from this pilot study set the foundation to further explore CBT treatment for childhood irritability. Although the therapy is not yet ready for clinical practice, it offers one of the few evidence-based treatments for this frequent and impairing childhood disorder. The researchers plan to test and refine the exposure therapy in larger, more controlled clinical trials to advance treatment for children with severe irritability and their families.
Reference
Naim, R., Dombek, K., German, R. E., Haller, S. P., Kircanski, K., & Brotman, M. A. (2023). An exposure-based cognitive–behavioral therapy for youth with severe irritability: Feasibility and preliminary efficacy. Journal of Clinical Child & Adolescent Psychology. https://doi.org/10.1080/15374416.2023.2264385
