Noninvasively Stimulating Deep Brain Areas to Treat Depression Symptoms
• Research Highlight
Changes in brain activity are known contributors to the risk for depression. Can altering the activity between brain areas also offer a treatment for this common but serious mood disorder?
A neuroimaging study funded by the National Institute of Mental Health explored whether a brain stimulation therapy known as repetitive transcranial magnetic stimulation (rTMS) could target regions deep in the brain via their surface connections. The study offers new evidence that stimulating deeper brain areas can reduce depression symptoms and identifies a possible target for improved depression treatment.
What area of the brain did the researchers look at?
Researchers led by Desmond Oathes, Ph.D. , and Kristin Linn, Ph.D. , at the Center for Brain Imaging and Stimulation (CBIS) at the University of Pennsylvania Perelman School of Medicine studied an area of the brain called the subgenual anterior cingulate cortex, or sgACC.
Located in the brain’s prefrontal cortex, the sgACC is important for regulating difficult emotions like sadness and anxiety and has been linked to the risk for depression and other mood disorders. It is part of an emotion-related brain network that includes other sites in the prefrontal cortex. In previous studies, people with depression were more likely to improve if rTMS was applied to prefrontal sites highly connected to the sgACC, spotlighting that connection as a promising target for rTMS treatment.
How did the researchers treat depression?
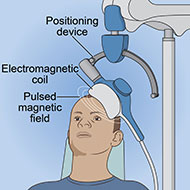
rTMS is a precise and noninvasive brain stimulation tool used to treat depression and other mental disorders. Brain stimulation therapies can play a critical role when other depression treatments like medication and therapy have not worked.
rTMS can only directly stimulate the outer layers of the brain. However, brain regions are highly connected, allowing them to support complex functions like emotion. It also suggests that reaching deeper brain areas, such as the sgACC, might be possible by stimulating surface areas linked to them. To accomplish this, researchers have used imaging techniques like functional MRI (fMRI) to guide rTMS to deeper subcortical brain regions.
In a prior study , the research team used rTMS to successfully target the amygdala—a deep brain area linked to anxiety and fear. However, the antidepressant effects of rTMS are not fully understood, and researchers have yet to determine the brain areas to target for the greatest clinical improvement.
What did the researchers do in this study?
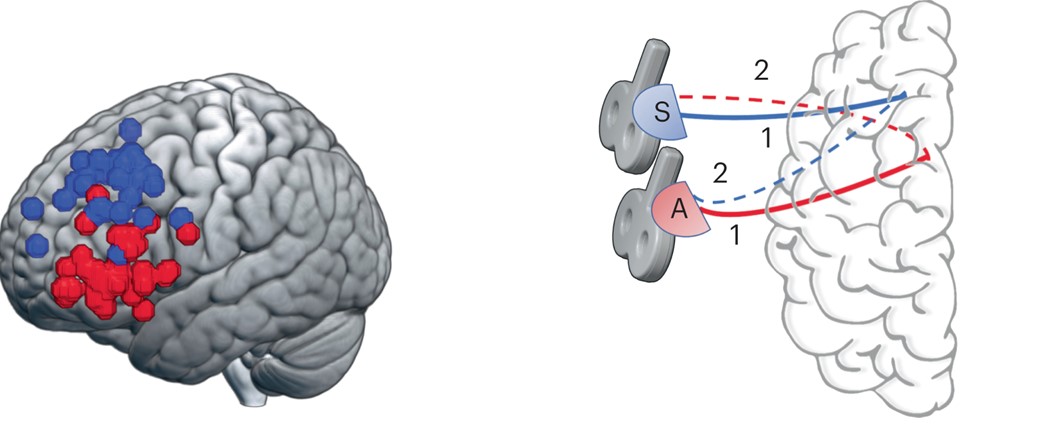
Thirty-six adults (18–54 years) diagnosed with depression and not taking any psychiatric medications participated in this study. In an initial session, the researchers used fMRI to map each participant’s connection from the prefrontal cortex to the sgACC. They used that data to determine the exact stimulation site for each participant’s rTMS treatment to target their sgACC.
All participants then completed three days of rTMS treatment sessions. Before and after treatment, participants completed a short round of rTMS, followed by single pulses of TMS during an fMRI brain scan. Taking the unique step of stimulating the brain with TMS while fMRI data were being recorded allowed the researchers to capture the brain’s response to rTMS and how it changed during treatment.
Clinicians also rated participants’ depression symptoms before and after the rTMS sessions to determine if their symptoms improved and, if so, whether that improvement was related to their sgACC response.
Did the rTMS treatment change the sgACC response or depression symptoms?
The researchers successfully used rTMS to stimulate the sgACC via its connections to surface brain areas. This finding indicates that fMRI can be used to guide rTMS to deeper brain regions.
After the 3-day rTMS treatment, participants' depression symptoms improved by 34%, and their anxiety symptoms improved by 32%. This change in symptoms corresponded to changes in sgACC activity, establishing a therapeutic role for rTMS in treating depression through this pathway.
Importantly, the change in depression symptoms was predicted by the initial sgACC response to TMS in the scanner. Participants with a stronger negative sgACC response to rTMS at pre-treatment went on to have a larger decrease in depression symptoms at post-treatment. The pre-treatment sgACC response was not related to the change in anxiety symptoms, suggesting the specificity of this pathway to depression.
A larger improvement in depression symptoms was also associated with a more positive (indicating a weaker) post-treatment sgACC response. Consistent with previous studies, the researchers propose that a weakening of the connection from the prefrontal cortex to the sgACC had a beneficial effect on depression symptoms in this sample of adults with the disorder.
What do the results of this study mean?
This study offers critical insight into how rTMS engages neural circuits in the brain to contribute to depression improvement, emphasizing an important link between the location of brain stimulation and the change in depression symptoms. Notably, the researchers targeted and modulated the depression-related brain circuit using a safe, noninvasive means in both fMRI and rTMS.
According to the researchers, the findings are some of the strongest evidence to date that subgenual connectivity in the brain is a marker of antidepressant response. The identified pathway from the sgACC to the prefrontal cortex responded to rTMS and provided fast-acting relief from depression symptoms. Incorporating fMRI-based brain mapping into rTMS sessions could make it possible to map outer brain areas accessible by rTMS to then stimulate deeper regions underlying depression and other disorders. This could eventually lead to more personalized or effective treatments for many mental disorders.
Although still preliminary, the possible clinical implications of this study are broad. A next step for the researchers is to replicate the findings in larger clinical trials of diverse people with and without depression and in people diagnosed with other mental disorders, such as post-traumatic stress disorder (PTSD). Knowing that numerous brain areas and networks play a role in the clinical effects of rTMS, the researchers also plan to examine other brain areas to enhance the treatment and better understand when, how, and for whom rTMS works best.
Reference
Oathes, D. J., Duprat, R. J.-P., Reber, J., Liang, X., Scully, M., Long, H., Deluisi, J. A., Sheline, Y. I., & Linn, K. A. (2023). Non-invasively targeting, probing and modulating a deep brain circuit for depression alleviation. Nature Mental Health, 1, 1033–1042. https://doi.org/10.1038/s44220-023-00165-2
