RAISE-ing the Standard of Care for Schizophrenia: The Rapid Adoption of Coordinated Specialty Care in the United States
• Feature Story • 75th Anniversary
At a Glance
- First-episode psychosis is often an early indicator of schizophrenia, which can have lifelong and debilitating consequences without treatment.
- NIMH initiated the Recovery After an Initial Schizophrenia Episode (RAISE) research initiative to investigate a new way of treating early psychosis called coordinated specialty care (CSC).
- Results showed that CSC can reduce the burden of first-episode psychosis and improve the lives of people with schizophrenia.
- CSC is a research-to-practice victory that charts the journey of schizophrenia treatment from dire beginnings to action-oriented research to broad implementation in the U.S. health care system.
- RAISE inspired a revolution in treating schizophrenia, leading to the rapid growth of CSC programs nationwide and increased access to high-quality care for thousands of Americans.
Young adulthood is a time of firsts: driving a car, living on your own, falling in love. But for some people, this period can include another milestone—their first episode of psychosis.
Psychosis is a loss of contact with reality in which a person’s thoughts and perceptions are disturbed. A first episode of psychosis often marks the onset of schizophrenia—a serious and potentially debilitating mental illness. Symptoms of first-episode psychosis can include hallucinations, delusions, unusual ways of thinking, incoherent speech, and inappropriate behavior. This complex range of symptoms is not only distressing for the person experiencing them but also challenging to treat successfully.
However, early care is effective at offsetting these symptoms. Research strongly supports the first few years after the start of psychotic symptoms as a critical period for intervention because this is when the steepest decline in health usually occurs, and the greatest therapeutic response can be achieved.
In contrast, if left untreated, schizophrenia often becomes more complicated and, over time, can impair physical and mental health, disrupt work or school, strain relationships with family or friends, and more, creating the conditions for unemployment, homelessness, incarceration, and long-term disability. And the longer symptoms go untreated , the greater the risk of these problems occurring. For this reason, the World Health Organization recommends a delay of no more than 90 days between the start of psychosis symptoms and specialized treatment. Simply put, early intervention is critical.
Unfortunately, in the United States, effective care for psychosis was almost nonexistent 20 years ago. Instead, people with early psychosis were met with long treatment delays, often going years without care after symptoms began. And the care that did exist was hard to access and had limited treatment goals that focused primarily on stabilizing symptoms and seldom on promoting recovery in work, school, or relationships.
According to Robert Heinssen, Ph.D., director of the NIMH Division of Services and Intervention Research at the time, studies “painted an alarming picture of treatment delays, questionable medication practices, and inadequate attention to medical comorbidities.” As a result, young people with schizophrenia often faced poor prospects for recovery, including frequent relapses, significant long-term disability, and a shorter lifespan of up to 25 years , alongside social isolation and limited work and school opportunities.
Yet it didn’t have to be that way. Years of research in academic settings and other countries showed that intervening quickly after psychotic symptoms began with comprehensive, evidence-based care led to dramatically better outcomes. However, no studies of comprehensive specialized care for early psychosis had been conducted in the United States. After years of insufficient schizophrenia treatment, the National Institute of Mental Health (NIMH), part of the National Institutes of Health (NIH), heeded the call for more effective early psychosis care by initiating a series of groundbreaking research studies.
Road to discovery
Coordinated specialty care
NIMH took note of what other countries were doing to effectively treat psychosis and combined them into a package of services that, in the United States, became known as coordinated specialty care (CSC).
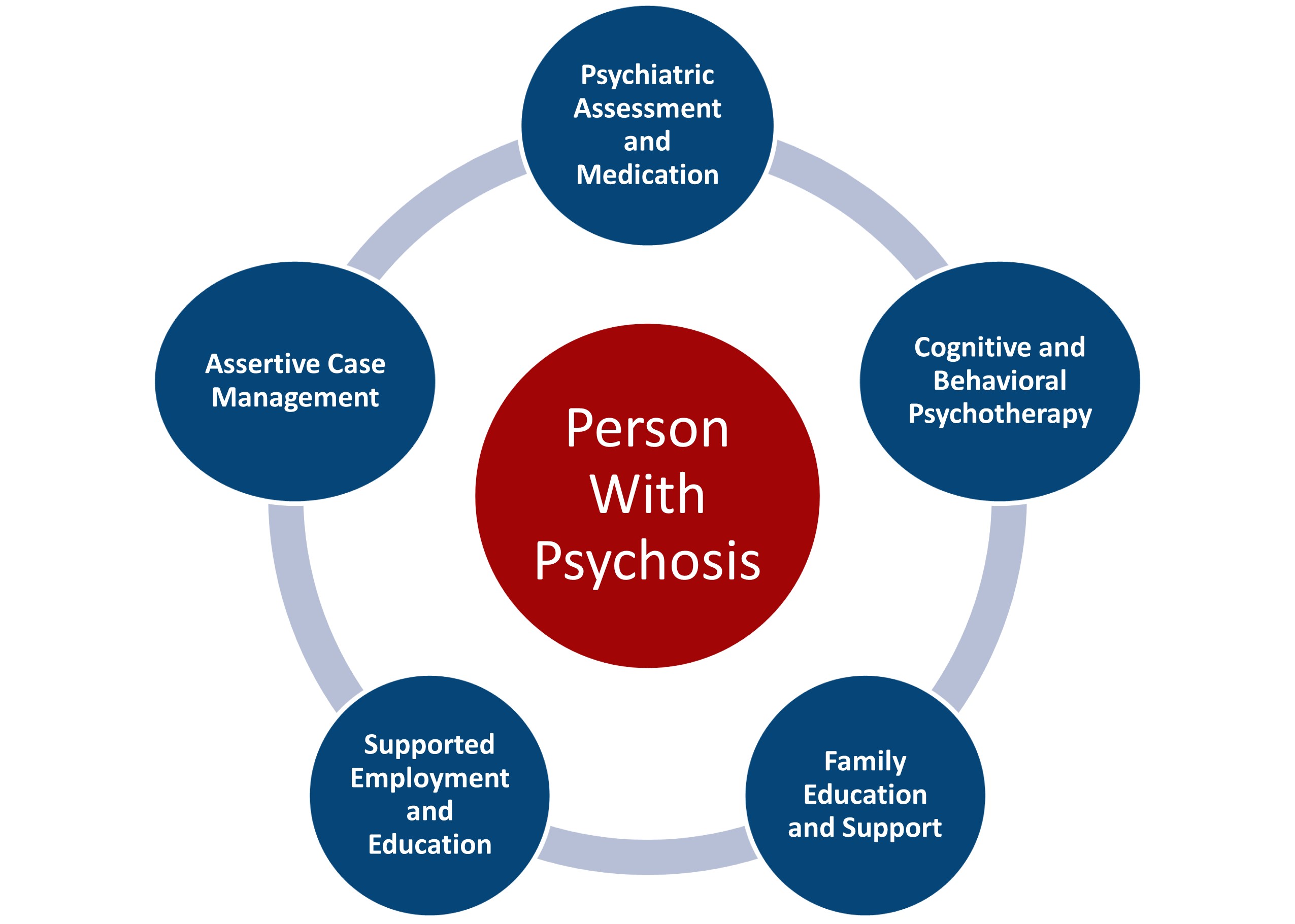
CSC is a multi-element, recovery-oriented, and patient-centered approach to treating early psychosis. Emphasis is on easy access to care and shared decision-making among a team of specialists who work with the patient and their family to create an individualized treatment plan reflecting their unique needs. Success is measured not only in reducing psychosis symptoms through psychotherapy and medication but in enhancing family support and teaching life skills to promote overall recovery and participation in work or school.
Recovery After an Initial Schizophrenia Episode research studies
NIMH launched the Recovery After an Initial Schizophrenia Episode (RAISE) research initiative in June 2008 to rigorously evaluate the effectiveness of CSC in community settings in the United States. At the finish line, NIMH aimed to have a comprehensive system of care for schizophrenia that would prevent future episodes of psychosis, avoid long-term disability, and improve recovery trajectories, all while reducing costs to the person and society.
RAISE presented a bold challenge to schizophrenia researchers: Plan intervention studies that would generalize to real-world health centers and support the rapid growth of effective treatments nationwide. This was an ambitious aim that would require ambitious research to achieve. As described by NIMH Director Dr. Joshua A. Gordon, “NIMH rose to the challenge by launching a groundbreaking research project that upended the traditional clinical trial model through an emphasis on partnerships among researchers, patients, families, clinicians, and administrators and using deployment-focused studies designed to speed the roll-out of effective solutions.”

By 2009, NIMH had selected two innovative, complementary projects to test the feasibility, effectiveness, and scalability of early intervention CSC services for first-episode psychosis. These projects, led by John Kane, M.D., and Lisa Dixon, M.D., would open the door to a revolution in how early serious mental illness is treated in this country.
As the driving force behind RAISE, Dr. Heinssen recognized the revolutionary potential of these studies before they started. “Each study capitalized on decades of scientific accomplishment to answer NIMH’s call for developmentally informed, comprehensive, patient-centered interventions to meet the needs of youth experiencing the earliest stages of serious mental illness.”
However, NIMH had to see if CSC could be used to effectively treat early psychosis within the realities of the U.S. health care system. Clinicians, administrators, and health agencies needed to know how such evidence-based treatment might translate into real-world mental health settings, accounting for such common barriers as workforce shortages and a decentralized health care system.
The first study—the RAISE Early Treatment Program Study (RAISE-ETP) —asked whether:
- CSC worked better than typical care for treating early psychosis in community clinics
- It was feasible to implement and sustain CSC programs in real-world settings
To investigate these questions, the researchers randomly assigned 34 community clinics to deliver a CSC intervention called NAVIGATE or provide typical care as usual. They then looked at how the two groups compared on a range of meaningful clinical and behavioral outcomes.
Developed with support from NIMH, NAVIGATE was a comprehensive CSC program designed to provide early and effective treatment to people with first-episode psychosis. The name “NAVIGATE” conveyed the mission of helping people with first-episode psychosis and their families successfully navigate the early course of illness and access needed services in the mental health system. The program consisted of medication management plus three psychosocial components designed to help people achieve their life goals: individual resilience training, supportive employment and education, and family therapy.
The second study—the RAISE Implementation and Evaluation Study (RAISE-IES) —examined:
- Barriers to the expansion of CSC treatment
- Effective ways for clinics to start using CSC treatment
Through partnerships with state commissioners of mental health in New York and Maryland , RAISE-IES offered an in-depth examination of potential barriers to CSC. More importantly, the researchers designed tools to overcome those barriers to make sure high-quality treatment could be sustained in mental health clinics in the real world.
Results of RAISE research
RAISE-ETP showed that CSC could be effectively used in mental health settings in the United States, that clinicians in those settings could be trained in the principles of evidence-based early psychosis care, and that such care led to greater improvements in symptoms and recovery compared to standard early psychosis treatment.
"Reframing how care was provided through such means as collaborative decision-making between patients and clinicians led to patients being more engaged in treatment and having better adherence to medication. In turn, patients experienced remarkable improvements that far exceeded what we saw in typical care settings,” said Dr. Heinssen. “CSC treatment improved their symptoms, outcomes for work and school, interpersonal relationships, and overall quality of life.”

An even more striking finding came when researchers looked at how long people had waited before entering treatment. It turned out that patients who received CSC treatment within 18 months of their first psychotic episode experienced a much greater improvement in their psychosis symptoms and quality of life compared to those seen after 18 months. Thus, the positive benefits of CSC treatment multiplied when people received care earlier.
“Doing the right thing—and doing it at the right time—that was the key finding,” stressed Dr. Heinssen.
In RAISE-IES, researchers identified potential barriers to implementing CSC and came up with easy-to-use tools and practical solutions to overcome those barriers. For instance, based on stakeholder input, they developed a suite of planning, training, management, assessment, and service delivery tools that clinics could use to implement CSC and ensure that care delivered across clinics was consistent, effective, and patient-focused.
In 2013, state mental health authorities in New York and Maryland announced plans for state-wide early intervention services based on the CSC model, foreshadowing the nationwide expansion of CSC programs to come. Nowadays, CSC is the recommended treatment for patients with schizophrenia who are experiencing a first episode of psychosis, per “The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia .”
Advancing the science
CSC spreads across the United States
RAISE spearheaded a revolution in treating early psychosis that resulted in making CSC the standard of care for schizophrenia in this country.
As described by Susan Azrin, Ph.D., chief of the Early Psychosis Services Research Program at NIMH, “RAISE not only contributed to the creation of a new way to organize and deliver treatment, but it produced findings that changed the standard of practice for early schizophrenia treatment in the United States.”
RAISE transformed the outlook for young people in the early stages of schizophrenia in this country. And, as the driving force in conceptualizing, implementing, and funding the studies, NIMH led this transformation in schizophrenia treatment from simply managing symptoms to promoting recovery and encouraging participation in work and school.
The shift that RAISE inspired in the youth mental health landscape prompted Congress to invest majorly in evidence-based, community-focused early psychosis treatment.
In 2014, Congress designated $25 million to the Substance Abuse and Mental Health Services Administration (SAMSHA)’s Community Mental Health Block Grant program. The program supports evidence-based treatments that address the needs of people with early serious mental illnesses, including psychotic disorders. The set-aside funding doubled to $50 million in 2016 and has increased every year since, resulting in a total investment in early psychosis care of nearly $430 million as of 2021.
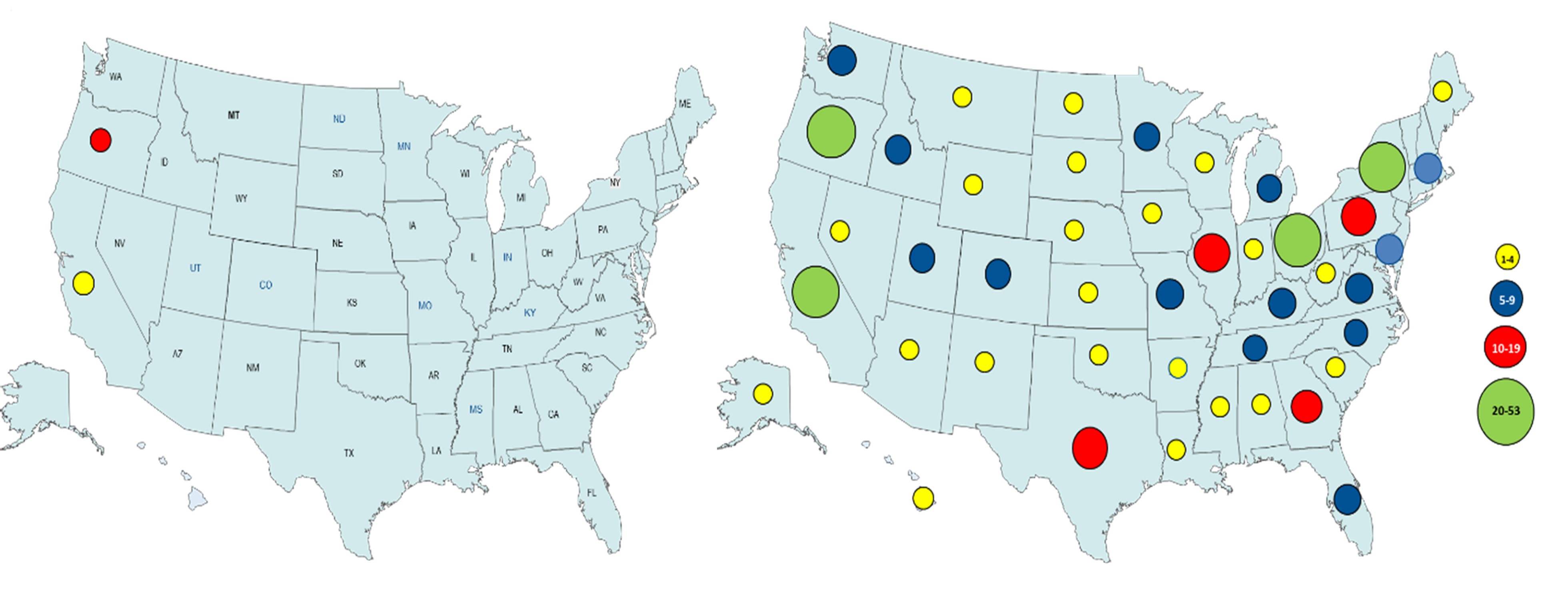
Federal investment in CSC has had a significant impact. In 2020, SAMHSA reported to Congress that 340 CSC programs for first-episode psychosis operated in all 50 states—a 30-fold increase in early psychosis programs compared to the years before RAISE. Most programs followed the models pioneered in RAISE, and the remainder followed the principles of person-centered, multi-component treatment tested in the research program. Likewise, the number of people treated in these programs has increased steadily over time, with over 22,000 youth receiving such care in 2020, compared to several hundred a decade earlier.
NIMH continues to advance CSC treatment

In 2019, NIMH leveraged the widespread expansion of CSC programs into the Early Psychosis Intervention Network (EPINET) . EPINET is a pioneering effort to adapt the principles and methods of learning health care to promote advances in early intervention, patient recovery, and scientific discovery. It operates via a national network of CSC clinics supported by a data coordinating center.
EPINET links over 100 CSC programs serving thousands of people with early schizophrenia in 17 states. Using a shared battery of standardized measures, the clinics track patient outcomes and provide information on national trends to help improve schizophrenia care. EPINET researchers address critical needs, such as reducing treatment delays, treating substance use, preventing suicide, and delivering remote care. Patients, families, health care providers, administrators, and others can also partner with EPINET to conduct or participate in large-scale, practice-based research aimed at enhancing the quality of CSC programs.
By supporting the continual improvement of CSC and fostering lifelong success for people with schizophrenia, EPINET represents the next chapter in NIMH’s “science-to-service story” of recovery in people with early serious mental illnesses. “Because of EPINET, tens of thousands of young people nationwide with early schizophrenia now receive CSC services and experience substantially improved quality of life as a result,” said Dr. Azrin.
The journey from the RAISE studies to EPINET to the widespread adoption of CSC treatment epitomizes an NIH success story that NIMH was at the heart of.
“A strategic approach to applying research findings transformed mental health care in the United States,” said Dr. Gordon. “Through RAISE, NIMH catalyzed CSC into the standard of care for early psychosis and ensured that young people with schizophrenia in this country would have access to early, evidence-based, and comprehensive care essential for their future success.”
Publications
Azrin, S. T., Goldstein, A. B., & Heinssen, R. K, (2015). Early intervention for psychosis: The Recovery After an Initial Schizophrenia Episode project. Psychiatric Annals, 45(11), 548–553. https://doi.org/10.3928/00485713-20151103-05
Browne, J., Penn, D. L., Meyer-Kalos, P. S., Mueser, K. T., Estroff, S. E, Brunette, M. F., Correll, C. U., Robinson, J., Rosenheck, R. A., Schooler, N., Robinson, D. G., Addington, J., Marcy, P., & Kane, J. M. (2017). Psychological well-being and mental health recovery in the NIMH RAISE early treatment program. Schizophrenia Research, 185, 167–172. https://doi.org/10.1016/j.schres.2016.11.032
Dixon, L. B., Goldman, H. H., Bennett, M. E., Wang, Y., McNamara, K. A., Mendon, S. J., Goldstein, A. B., Choi, C.-W. J., Lee, R. J., Lieberman, J. A., & Essock, S. M. (2015). Implementing coordinated specialty care for early psychosis: The RAISE Connection Program. Psychiatric Services, 66(7), 691–698. https://doi.org/10.1176/appi.ps.201400281
Essock, S. M., Goldman, H. H., Hogan, M. F., Hepburn, B. M., Sederer, L. I., & Dixon, L. B. (2015). State partnerships for first-episode psychosis services. Psychiatric Services, 66(7), 671–673. https://doi.org/10.1176/appi.ps.201400117
Goldstein, A. B., Heinssen, R. K., & Azrin, S. T. (2015). Accelerating science-to-practice for early psychosis. Psychiatric Services, 66(7), 665. https://doi.org/10.1176/appi.ps.660708
Heinssen, R. K., & Azrin, S. T. (2022). A national learning health experiment in early psychosis research and care. Psychiatric Services, 73(9), 962–964. https://doi.org/10.1176/appi.ps.20220153
Insel, T. R. (2016). RAISE-ing our expectations for first-episode psychosis. American Journal of Psychiatry, 173(4), 311–312. https://doi.org/10.1176/appi.ajp.2015.15091204
Kane, J. M., Robinson, D. G., Schooler, N. R., Mueser, K. T., Penn, D. L., Rosenheck, R.A., Addington, J., Brunette, M. F., Correll, C. U., Estroff, S. E., Marcy, P., Robinson, J., Meyer-Kalos, P. S., Gottlieb, J. D., Glynn, S. M., Lynde, D. W., Pipes, R., Kurian, B. T.,Miller, A. L. … Heinssen, R. K. (2016). Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. American Journal of Psychiatry, 173(4), 362–372. https://doi.org/10.1176/appi.ajp.2015.15050632
Kane, J. M., Schooler, N. R., Marcy, P., Correll, C. U., Brunette, M. F., Mueser, K. T., Rosenheck, R. A., Addington, J., Estroff, S. E., Robinson, J., Penn, D. L., & Robinson, D. G. (2015). The RAISE Early Treatment Program for first-episode psychosis: Background, rationale, and study design. The Journal of Clinical Psychiatry, 76(3), 240–246. https://doi.org/10.4088/JCP.14m09289
Keepers, G. A., Fochtmann, L. J., Anzia, J. M., Benjamin, S., Lyness, J. M., Mojtabai, R., Servis, M., Walaszek, A., Buckley, P., Lenzenweger, M. F., Young, A. S., Degenhardt, A., & Hong, S. H. (2020). The American Psychiatric Association practice guideline for the treatment of patients with schizophrenia. American Journal of Psychiatry, 177(9), 868–872. https://doi.org/10.1176/appi.ajp.2020.177901
Marino, L., Nossel I., Choi, J. C., Nuechterlein, K., Wang, Y., Essock, S., Bennett, M., McNamara, K., Mendon, S., & Dixon, L. (2015). The RAISE Connection Program for early psychosis: Secondary outcomes and mediators and moderators of improvement. The Journal of Nervous and Mental Disease, 203(5), 365–371. https://doi.org/10.1097/NMD.0000000000000293
Mueser, K. T., & Cook, J. A. (2014). Rising to the challenge of first episode psychosis: The NIMH Recovery After Initial Schizophrenia Episode (RAISE) initiative [Editorial]. Psychiatric Rehabilitation Journal, 37(4), 267–269. https://doi.org/10.1037/prj0000108
Mueser, K. T., Penn, D. L., Addington, J., Brunette, M. F., Gingerich, S., Glynn, S. M., Lynde, D. W., Gottlieb, J. D., Meyer-Kalos, P., McGurk, S. R., Cather, C., Saade, S., Robinson, D. G., Schooler, N. R., Rosenheck, R. A., & Kane, J. M. (2015). The NAVIGATE program for first-episode psychosis: Rationale, overview, and description of psychosocial components. Psychiatric Services, 66(7), 680–690. https://doi.org/10.1176/appi.ps.201400413
National Alliance on Mental Illness. (2017). First episode psychosis programs: A guide to state expansion. https://www.nami.org/getattachment/Extranet/Advocacy/FEP-State-Advocacy-Toolkit/FEP-State-Advocacy-Guide.pdf
Powell, A. L., Hinger, C., Marshall-Lee, E. D., Miller-Roberts, T., & Phillips, K. (2021). Implementing coordinated specialty care for first episode psychosis: A review of barriers and solutions. Community Mental Health Journal, 57(2), 268–276. https://doi.org/10.1007/s10597-020-00644-1
Read, H., & Kohrt, B. A. (2022). The history of coordinated specialty care for early intervention in psychosis in the United States: A review of effectiveness, implementation, and fidelity. Community Mental Health Journal, 58(5), 835–846. https://doi.org/10.1007/s10597-021-00891-w
Rosenheck, R., Leslie, D., Sint, K., Lin, H., Robinson, D. G., Schooler, N. R., Mueser, K. T., Penn, D. L., Addington, J., Brunette, M. F., Correll, C. U., Estroff, S. E., Marcy, P., Robinson, J., Severe, J., Rupp, A., Schoenbaum, M., & Kane, J. M. (2016). Cost-effectiveness of comprehensive, integrated care for first episode psychosis in the NIMH RAISE early treatment program. Schizophrenia Bulletin, 42(4), 896–906. https://doi.org/10.1093/schbul/sbv224
Stetka, B. S. Kane, J. M., Mueser, K. T., Robinson, D. G., & Heinssen, R. K. (2016). Treating early psychosis in the 'real world.' Medscape Psychiatry. https://www.medscape.com/viewarticle/866156_1
Learn more
- Early Assessment and Support Alliance (EASA)
- Early Psychosis Intervention Network (EPINET)
- NAVIGATE
- OnTrackNY
- Specialized Treatment Early in Psychosis (STEP)
- Congressional legislation: Consolidated Appropriations Act, 2014, H.R.3547
- NIH case study: Rapid Translation of Science to Real-World Practice: Coordinated Specialty Care Treatment Programs for Early Schizophrenia
- NIH Director’s Blog: Study May RAISE Standard for Treating First Psychotic Episode
- NIMH Director’s Message: Highlighting Services and Effectiveness Research at NIMH
- NIMH fact sheet: Understanding Psychosis
- NIMH health information: Schizophrenia
- NIMH highlighted research initiative: Recovery After an Initial Schizophrenia Episode (RAISE)
- NIMH report: Evidence-Based Treatments for First Episode Psychosis: Components of Coordinated Specialty Care
- NIMH statistics: Schizophrenia
Science news
- NIH news release: Increased Health Risks Linked to First-Episode Psychosis
- NIH news release: Major NIMH Research Project to Test Approaches to Altering the Course of Schizophrenia
- NIH news release: Medications for Patients With First-Episode Psychosis May Not Meet Guidelines
- NIH news release: Team-Based Treatment Is Better for First-Episode Psychosis
- NIH news release: Team-Based Treatment for First Episode Psychosis Found to Be High Value
- NIH Research Matters: Targeting Health Risks in Early Stages of Schizophrenia
- NIMH Science News About Schizophrenia
- NIMH press release: NIH Announces Funding Awards for National Early Psychosis Learning Community
- NIMH research highlight: NIH Initiative Expands Access to Resources for Early Psychosis Treatment and Research
- NIMH science update: NIMH RAISE Project Makes Progress as Teams Refine Research Approaches
- NIMH science update: Psychosis Treatment Program Expands in New York
