Archived Content
The National Institute of Mental Health archives materials that are over 4 years old and no longer being updated. The content on this page is provided for historical reference purposes only and may not reflect current knowledge or information.
Hyperconnectivity in a Brain Circuit May Predict Psychosis
• Science Update
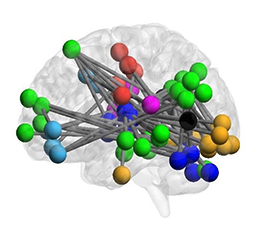
National Institute of Mental Health (NIMH)-funded scientists have discovered a pattern in the way a brain circuit works that may help predict the onset of psychosis. High levels of chatter, or “hyperconnectivity,” in a circuit involving the cerebellum, thalamus, and cortex emerged as a potential “neural signature” in a functional magnetic resonance imaging (fMRI) study by Tyrone Cannon, Ph.D. of Yale University and colleagues.
The degree of hyperconnectivity within this circuit predicted the length of time it took for an individual to convert from a state of risk to full psychosis – hallucinations, delusions, and disorganized thought and behavior. The researchers also found this same pattern of hyperactivity in a separate group of individuals with schizophrenia.
Early detection of these atypical neural connections could potentially find application as a neuroimaging biomarker to predict the onset of symptoms and in the development of preventive interventions, suggest researchers.
The “cerebello-thalamo-cortical” network detected in the new study is linked to neural systems known to be more widely associated with psychotic symptoms and implicated in cognitive deficits in individuals with psychosis, including those with schizophrenia.
Previous imaging studies have identified brain differences in individuals suspected of being at high risk for psychosis, based on symptoms and declines in their life functioning. Yet, findings have varied across studies, depending on the neuroimaging paradigm used – for example, whether participants were at rest or performing cognitive tasks.
In the new study, the researchers examined neural connectivity across a variety of fMRI paradigms to analyze signals that represented stable connectivity. A measure emerged that accounted for 70 percent of the variance when the data were examined together. Based on this measure, the group at risk for psychosis showed increased connectivity relative to the control group. The researchers saw the same pattern of Increased connectivity in individuals with schizophrenia. It exceeded the pattern seen in other disorders, such as attention-deficit/hyperactivity disorder (ADHD) and bipolar disorder.
The difference in connectivity was correlated with disorganization symptoms (e.g., incoherent and illogical thoughts) in individuals at risk for psychosis, and predicted the length of time to conversion to full psychosis. This hyperconnectivity may reflect the brain exerting more effort in an attempt to compensate for an impaired ability to coordinate thoughts and behaviors and/or a “downstream” consequence of changes in a key brain chemical messenger system.
In addition to potential clinical applications for identifying people who may benefit from early intervention, the findings may also hold clues to underlying brain mechanisms involved in schizophrenia. The findings, reported in Nature Communications, were part of the NIMH-funded North American Prodromal Longitudinal Study (NAPLES-2) , a multisite study of a large sample of individuals at elevated risk for developing psychosis and healthy comparison participants. Limitations include a low rate of conversion to full psychosis (19 out of 182 high-risk individuals).
For more information, see Yale University’s news release:
Early warning sign of psychosis detected
Reference
Cerebello-thalamo-cortical hyperconnectivity as a state-independent functional neural signature for psychosis prediction and characterization. Cao H, Chén OY, Chung Y, Forsyth JK, McEwen SC, Gee DG, Bearden CE, Addington J, Goodyear B, Cadenhead KS, Mirzakhanian H, Cornblatt BA, Carrión RE, Mathalon DH, McGlashan TH, Perkins DO, Belger A, Seidman LJ, Thermenos H, Tsuang MT, van Erp TGM, Walker EF, Hamann S, Anticevic A, Woods SW, Cannon TD. Nat Commun. 2018 Sep 21;9(1):3836. doi: 10.1038/s41467-018-06350-7. PMID: 30242220
Grants
MH081902 , MH066286 , MH081857 , MH82022 , MH066134 , MH081944 , MH066069 , MH076989 , MH081928 , MH081988
