FY2025 Budget – Congressional Justification
National Institute of Mental Health
CONGRESSIONAL JUSTIFICATION FY 2025
National Institutes of Health
Department of Health and Human Services
- Director’s Overview
- IC Fact Sheet
- Major Changes
- Budget Mechanism Table
- Appropriations Language
- Summary of Changes
- Budget Graphs
- Organization Chart
- Budget Authority by ActivityTable
- Justification of Budget Request
- Appropriations History
- Authorizing Legislation
- Amounts Available for Obligation
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
General Notes
- FY 2024 Enacted levels cited in this document are based on the Continuing Resolution in effect at the time of budget preparation (Public Law 118-35) and do not include HIV/AIDS transfer.
- Detail in this document may not sum to the subtotals and totals due to rounding.
Director’s Overview

M.D., Ph.D.,
Director of NIMH
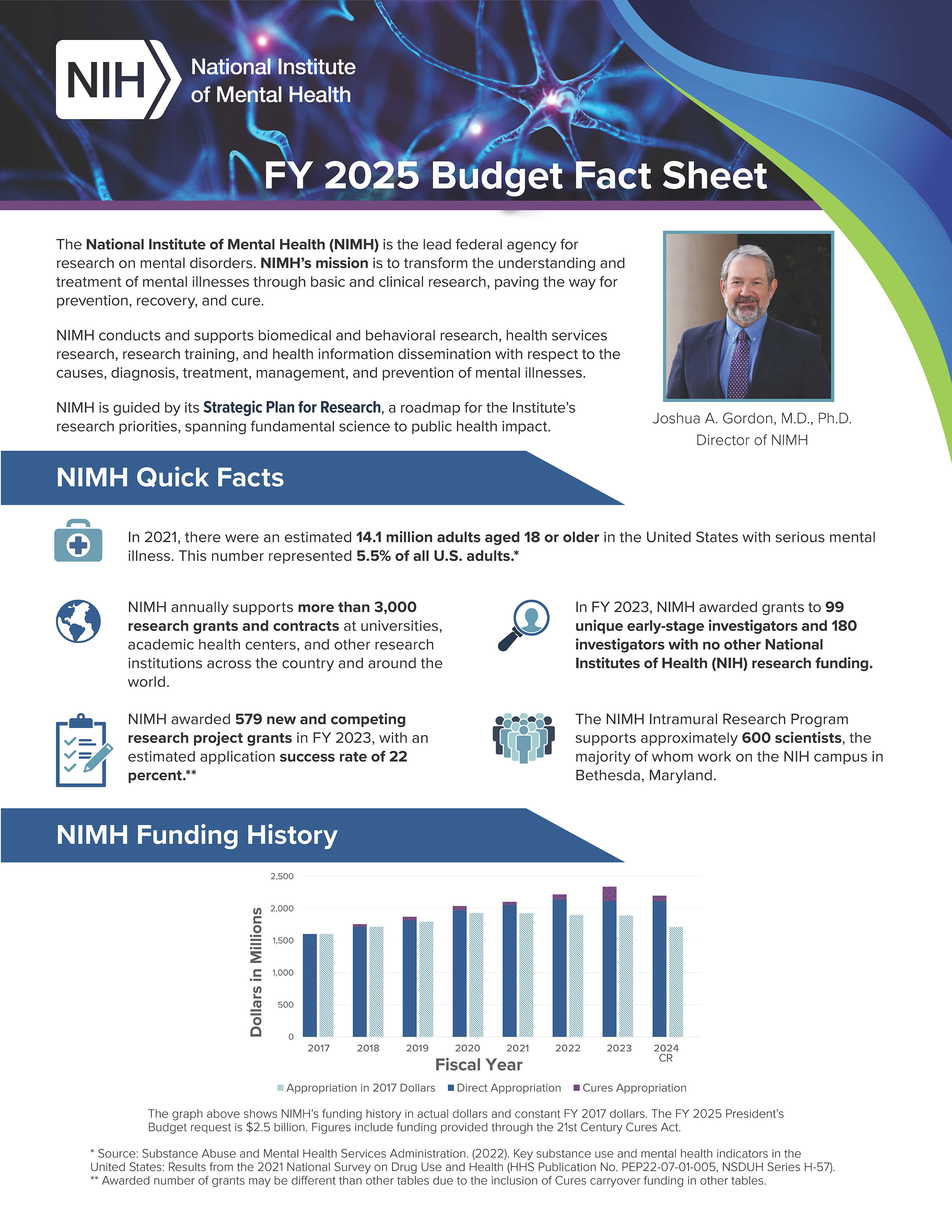
The National Institute of Mental Health (NIMH) is the lead federal agency for research on mental illnesses, with a mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure.
In the United States, an estimated 57.8 million adults struggle with a mental illness, which may be significantly impairing and life-threatening.1 Mental illnesses are the fifth leading cause of disability in the United States, accounting for 6.6 percent of all disability-adjusted life years.2 One of the most tragic outcomes of untreated mental illness is suicide. Provisional data indicate that suicide accounted for the loss of over 49,000 American lives in 2022 alone.3 Suicide is the second leading cause of death in youth and young adults aged 10-34, and the eleventh leading cause of death overall.4 In alignment with the Administration’s Unity Agenda5 and the White House Report on Mental Health Research Priorities,6 NIMH continues to lead the research response to the country’s ongoing mental health crisis, which disproportionately impacts certain populations such as veterans, caregivers, medical professionals, youth, sexual and gender minoritized groups and racially and ethnically minoritized groups. NIMH is committed to confronting the mental health crisis by supporting and conducting research that aims to transform how mental health is understood and how mental health treatments and services are accessed – not only in healthcare settings, but also in communities, educational settings, and other contexts.
NIMH is pursuing an ambitious and collaborative research agenda spanning basic, translational, and clinical research with the potential to improve clinical care over the short, medium, and long term. In May 2023, NIMH published an update to its Strategic Plan for Research.7 Most notably, the updated Plan emphasizes the institute’s commitment to funding research focused on reducing mental health disparities and promoting health equity. NIMH also published a new edition of the Strategic Plan Progress Report,8 which highlights significant accomplishments made during FY 2022 toward achieving the goals described in the Strategic Plan. These accomplishments reflect the institute’s sustained commitment to ensuring the relevance, timeliness, and real-world impact of the research that NIMH supports.
Looking back: Advances in understanding and treating mental illnesses
NIMH 75th Anniversary: Significant achievements and progress in improving the understanding and treatment of mental illnesses. In 1946, President Harry S. Truman signed the National Mental Health Act, which enabled the founding of NIMH. For 75 years, NIMH has remained committed to supporting research that transforms the understanding of mental illnesses and paves the way for prevention, recovery, and cure. NIMH-funded research has played a pivotal role in advancing basic science to decode the brain and behavior, developing groundbreaking treatments and therapies such as fast-acting antidepressants and cognitive behavioral therapy, and improving the quality and availability of evidence-based mental health care. NIMH is commemorating its 75th anniversary by reflecting on this research and what it has meant for people living with mental illnesses, their loved ones, their communities, and society at large. Continuing through September 2024, the institute is hosting a series of special events and sharing resources that highlight selected NIMH scientific accomplishments in mental health research and recognize those who have contributed to advancing the institute’s mission.9
Identification of genetic mechanisms of mental illnesses. Mental illnesses and other brain disorders are heritable and influenced by complex interactions among multiple genes and environmental factors. In recent decades, a data-rich research method, called genome-wide association, has emerged to try to identify specific genes involved in certain disorders. This and other technological advances have enabled tremendous progress in identifying genes that raise risk for mental illnesses. For example, NIMH-supported researchers studying individuals with bipolar disorder uncovered 64 risk loci – variations in the genome that raise risk for the disorder.10 The researchers then used a technique called fine mapping to identify 15 specific genes within these loci that most strongly predicted risk for bipolar disorder. In an NIMH-supported study focused on schizophrenia, researchers analyzed gene expression in post-mortem brain tissue to identify risk genes and gene networks – groups of genes that regulate each other’s expression or participate in the same biological functions.11 The researchers identified altered expression in 2,700 genes among subjects with schizophrenia, including changes specifically in the dopamine signaling system that could lead to a causal mechanism. The rapid growth of tools to identify risk genes has also led to significant advances in understanding other disorders of the brain, including malformations of cortical development and substance use disorders.12,13 Looking forward, more work is needed to better understand the biological functions affected by risk genes and to include greater ancestral diversity in genetics research, so that these advances can be translated into novel treatments that benefit all people.
Improving access to evidence-based treatment for postpartum depression (PPD): Zuranolone. In August 2023, the Food and Drug Administration (FDA) approved the synthetic neuroactive steroid zuranolone for the treatment of PPD, a serious mental illness that impacts approximately 1 in 9 people who give birth. Like its predecessor brexanolone,14 zuranolone represents a remarkable bench-to-bedside success story: it targets the same biological mechanism, which was gradually uncovered by multiple NIMH intramural scientists and NIMH-funded extramural investigators over several decades, and it acts rapidly to reduce the severity of depressive episodes in PPD. However, unlike brexanolone, which must be administered in specialized inpatient settings by health care providers as an intravenous infusion, zuranolone is taken orally as a pill, and this unique feature could significantly improve the accessibility of this treatment for people with PPD. Building on these advances, NIMH continues to support research focused on understanding the therapeutic mechanisms of neuroactive steroids,15 with the goal of developing even more effective and accessible treatments for mental illnesses.
Global mental health: Reducing the mental health treatment gap in low- and middle-income countries (LMICs). Mental disorders are a global concern and present shared opportunities and challenges to advance science across international borders. The burden of disease associated with mental disorders in LMICs is rising, with a substantial treatment gap for individuals who need but do not receive mental health treatment.16 Access to long-term psychosocial interventions and pharmacological management continue to be pervasively unavailable and/or inaccessible in most LMICs.17 NIMH’s Center for Global Mental Health Research facilitates research on the implementation, scaling-up, sustainable availability, and accessibility of mental health care in LMICs. Through these efforts, NIMH aims to expand the reach of evidence-based mental health interventions, build and sustain in-country capacity for conducting implementation research, and apply scientific evidence to develop mental health policies and programs.18
To address both immediate and long-term needs, NIMH supports research across a wide range of global mental health priorities, including reducing the risk of suicidal behaviors,19 improving the long-term management of mental health conditions,20 developing and testing interventions aimed at addressing social determinants of mental health,21 integrating mental healthcare in primary care,22 and developing and implementing metrics to improve quality of health care delivery.23 For instance, in efforts to close the mental health treatment gap in Sub-Saharan Africa, NIMH-supported researchers deployed a problem-solving therapy, locally termed the “Friendship Bench,” that is delivered by trained lay health workers and has been shown to be acceptable and effective in treating common mental illnesses.24,25 NIMH investments in effectiveness and implementation research in LMICs are producing innovative strategies for expanding access to mental health care and improving care quality and outcomes in a range of settings worldwide. Notably, some of these innovative strategies developed in LMICs – including the “Friendship Bench” strategy detailed above – are being adapted and deployed in the United States to address relevant domestic challenges.
Suppression of HIV among people with mental illnesses. HIV attacks the immune system by infecting a type of white blood cell in the body that is vital to fighting off infection. Antiretroviral treatment (ART) reduces the amount of HIV in an individual’s body, helping people with HIV live longer, healthier lives and reducing the risk of HIV transmission. Yet persistent barriers, including stigma, can delay the start of ART and reduce adherence among people who face significant health and social challenges. Long-acting injectable medications, administered every four or eight weeks, could help people overcome adherence barriers of daily oral ART. Currently, in the United States, this treatment is approved only for patients who have achieved viral suppression. In a recent study supported by NIMH, researchers provided participants with HIV who have historically had decreased access to ART, including people with mental illnesses, housing insecurity, and substance use disorders, with long-acting ART and evaluated each person’s health status on a biweekly basis. Importantly, participants did not have to be virally suppressed to start long-acting ART. Almost all participants achieved viral suppression, including those who were previously not virologically suppressed. The study findings indicate that long-acting injectable ART can benefit people who face treatment barriers and have been historically underserved.26
Brain mechanisms of stress and reward. Exposure to adverse experiences in early childhood significantly increases the risk of mental illnesses arising in adulthood and can also disrupt the formation of typical reward behaviors. To better understand the biological basis for these effects of early-life adversity, NIMH-supported researchers are investigating specific connections in the mammalian brain that control reward behaviors. Recently, the researchers discovered a novel connection between the basolateral amygdala–a brain region critical for forming associations between experiences and outcomes–and the nucleus accumbens, which is important for processing rewarding experiences. The researchers were able to selectively activate or silence this connection using chemical (chemogenetic) and light-based (optogenetic) methods in mice. When they activated the connection, the researchers found that mice showed impairments in reward behaviors, similar to the impairments observed in mice exposed to early-life stress. Conversely, when the researchers silenced this connection in mice that were previously exposed to early-life stress, they were able to restore typical reward behaviors.27 These findings are an important step toward understanding the biological mechanisms of stress-related mental illnesses such as post-traumatic stress disorder, potentially identifying novel targets for prevention and treatment.
Current efforts: Translating evidence to benefit people
Advancing learning health care: Early Psychosis Intervention Network (EPINET). Research has shown that early treatment of mental disorders increases the chance of successful recovery. Launched in 2019, EPINET is a learning health care system for early psychosis, aimed at enhancing coordinated specialty care to improve early identification, diagnosis, clinical assessment, intervention effectiveness, service delivery, and health outcomes. EPINET now has 8 regional scientific hubs and has enrolled approximately 4,000 participants from more than 100 clinics across 17 states.28,29 EPINET’s National Data Coordinating Center supports efforts to standardize, collect, and aggregate data to study the fidelity to the intervention, as well as the quality and treatment effectiveness.30 The EPINET research system is pioneering a learning health care approach to early psychosis intervention, incorporating measurement-based treatment that promotes scientific discovery and improvements in practice, and feeding back knowledge gained to participating clinics and supporting continuous quality improvement. To foster knowledge sharing and promote accessible early psychosis care resources, the EPINET National Data Coordinating Center launched a web portal,31 making the EPINET Core Assessment Battery available to all early psychosis care clinicians to assess key domains of early psychosis, recovery, and treatment.32
Addressing youth mental health disparities: Systems-level interventions for youth at risk of suicide. Between 2018 and 2021, suicide rates increased across nearly all racial and ethnic groups, including notable increases among American Indian/Alaska Native (26 percent), non-Hispanic Black (19 percent), and Hispanic (7 percent) individuals.33 Further, suicide remains a leading cause of death among youth. Provisional data from 2022 indicate an estimated 6,529 youth ages 10 to 24 died by suicide.34 Consistent with the NIMH Strategic Framework for Addressing Youth Mental Health Disparities,35 the institute is supporting research to address these disparities in suicide outcomes among youth, in part through the Practice-Based Suicide Prevention Centers. 36 These Centers are focused on developing, testing, and refining effective and scalable interventions at key points in the chain of care across diverse populations and settings. At one Center, investigators aim to expand the capacity of pediatric primary care to identify, refer, and manage youth at risk for suicide, particularly Black youth.37 Additionally, NIMH recently released a pair of funding opportunities that seek to support research to improve risk detection and intervention among youth and young adults from underserved populations who are at risk for suicide.38,39 This aligns with other NIMH efforts to meet the needs of underserved and high-risk populations, such as youth involved in the juvenile justice system. For instance, NIMH-supported researchers are working with community mental health providers to enhance the implementation of effective system-level interventions for juvenile justice-involved youth at risk for suicide.40
BRAIN Initiative Transformative Projects. The Brain Research Through Advancing Innovative Neurotechnologies® Initiative, or The BRAIN Initiative®, is revolutionizing our understanding of the human brain. This cross-cutting, multidisciplinary initiative encompasses 10 NIH institutes and centers, 4 additional federal agencies, and multiple private international organizations, going beyond the capability of any single institute or agency. The BRAIN Initiative announced three major transformative projects aimed at revolutionizing neuroscience research and how we treat brain disorders. The projects aim to characterize cell types in the human brain and uncover how the cells function in health, and ultimately, how they fail to function in disease. The three projects are: the BRAIN Initiative Cell Atlas Network (BICAN), focused on developing a comprehensive atlas of cell types in the mammalian brain; the BRAIN Initiative Connectivity across Scales Network (BRAIN CONNECTS), focused on developing and scaling up the tools necessary to complete a “wiring diagram” of an entire mammalian brain; and the Armamentarium for Precision Brain Cell Access, focused on developing new molecular and gene therapy strategies to study and treat human neural circuit disorders.41,42,43 BICAN builds on findings from the BRAIN Initiative Cell Census Network (BICCN), a collaboration of over 250 NIH-supported scientists at nearly 50 institutions across 3 continents.44 The coordinated efforts have resulted in foundational reference atlases for the mouse and, more recently, human and nonhuman primate brains.45,46 The BICCN findings have enabled advances in understanding the location and function of cell types, comparisons across species, and increasing the scale of technologies used to acquire these data. In addition, tools developed in the BICCN are already having an impact on clinical treatments today, as researchers utilize the technologies to gain insights into the cellular basis of Parkinson’s disease, Alzheimer’s disease, and substance use disorders at unprecedented resolution.47.48
Digital health interventions for suicide risk, PPD, and post-traumatic stress disorder. Technology offers promise to transform mental health services, providing new ways to access help and monitor treatment, as well as increase understanding of mental health and wellbeing. Digital health interventions aim to deliver treatment as a standalone intervention or as an adjunct to face-to-face treatments via a digital health platform. Digital health interventions have the potential to bridge the treatment gap by providing evidence-based interventions to many individuals who currently are unable to access treatments.49 NIMH’s Laboratories to Optimize Digital Health is an initiative that is funding several projects to test strategies to increase the reach, efficiency, and quality of digital mental health interventions which may impact mental health outcomes, including suicidal behaviors.50 Other NIMH-supported researchers are piloting technology-enabled services designed to treat depression in three distinct care settings: family medicine, a specialty obstetrics care setting for PPD, and a geriatrics service.51 Additionally, NIMH is supporting efforts to explore the role and impact of digital health interventions to address secondary health effects of the social, behavioral, and economic changes during and following the COVID-19 pandemic, particularly among health disparity groups and other vulnerable populations.52 Ongoing projects include evaluating text-based therapies for post-traumatic stress disorder and assessing the effectiveness of a digital platform to support health care workers’ mental health.53,54
Non-invasive brain stimulation to reduce auditory hallucinations in schizophrenia. Auditory hallucinations (hearing voices or noises without an external source) associated with schizophrenia can be persistent, debilitating, and difficult to treat. Auditory hallucinations may be rooted in altered brain activity in regions that control auditory function. In one ongoing NIMH-funded study, researchers aim to further develop Auditory Control Enhancement (ACE), a novel combination therapeutic intervention that combines psychotherapeutic behavioral training with targeted, non-invasive brain stimulation.55 The research team plans to examine the effects of ACE on brain regions associated with cognitive control using a variety of magnetic resonance imaging (MRI) measures, including changes in the measured magnetic field, the blood oxygenation level dependent response, cerebral blood flow, and electrophysiological measures. This research may provide preliminary data that can support future effectiveness trials of ACE as a novel approach with the potential to improve outcomes for individuals with treatment-resistant auditory hallucinations.
Biomarkers for early identification of autism spectrum disorder (ASD). ASD is a condition marked by unique behavioral, neural, and genetic signatures that may precede noticeable clinical symptoms. Researchers aim to identify potential biomarkers that could inform both research and clinical practice and help improve and expand early ASD screening efforts. Researchers supported by NIMH found that visual attention to dynamic geometric images may offer one such biomarker for a subset of toddlers with ASD.56 The researchers showed that, overall, toddlers with ASD spent more time looking at geometric images than social images (for example, images of other children). Toddlers with ASD who strongly preferred geometric images also had higher symptom scores, lower cognitive ability scores, and lower adaptive behavior scores than toddlers with ASD who strongly preferred images showing children.57 The fact that this geometric preference measure was accurate in a large, diverse, community-based sample that included toddlers with non-ASD developmental delays suggests the measure may have use in real-world clinical settings and in research as a biomarker for ASD. If validated in further studies, this measure may offer a low-cost, scalable tool for early screening and identification, as the task data can be obtained within 1 minute and is designed to be used prior to 24 months of age. This measure could therefore help some toddlers with ASD receive earlier diagnosis and access to services.
Looking forward: Filling the gaps in understanding and treatment
Precision Psychiatry Initiative: Innovation Funnel and Individually Measured Phenotypes to Advance Computational Translation in Mental Health (IMPACT-MH). Effective treatments for mental illnesses exist, yet tailoring treatment for individuals is often a trial-and-error process that can lead to unacceptable delays in receiving effective treatment. To address this pressing challenge, NIMH has launched the Precision Psychiatry Initiative, an ambitious research program that will target two parallel areas of need: biomarker development and precision assessments.
The biomarker development effort aims to deliver highly sensitive and specific biomarkers to guide treatment decisions for depression, as there is no current validated test (biological, physiological, or behavioral) that could inform treatment selection. This effort is divided into three phases, culminating in a large-scale prospective clinical trial with a focus on generalizability for underserved populations and populations experiencing health disparities. As part of this process, NIMH is applying the “innovation funnel” approach to support stage-gated, milestone-based projects to develop these highly sensitive and specific biomarkers to guide treatment decisions for depression. This innovation funnel involves a highly competitive, phased selection process that aims to accelerate the identification and development of a library of candidate tools. The long-term goal of this effort is to deliver validated clinical tools to enable patients to achieve rapid symptomatic relief and functional quality-of-life improvement.58
The precision assessment effort, IMPACT-MH, aims to support studies that use behavioral measures and computational methods to better predict patient prognosis and optimize treatment. These studies plan to combine data from behavioral tasks and measures with clinical records data to support individual-level prediction and clinical decision-making for mental disorders. Researchers plan to collect data from new clinical cohorts and/or existing data sets that have relevant measures, targeting specific clinical groupings (e.g., mood/anxiety disorders, disorders of behavioral regulation, or psychosis) and/or care delivery settings. IMPACT-MH aims to harness machine learning and other data-driven approaches to integrate data from behavioral assessments with clinically available data, with the goal of generating more precise, objective clinical signatures and improving mental health outcomes.59,60
Transforming the digital ecosystem: Technology and digital media impacts on mental health. While digital health technology is a growing platform that holds promise to expand and offer new ways to access mental health care, the potential harms of technology and digital media on health and development, particularly on youth mental health, must be considered and better understood. In May 2023, the U.S. Surgeon General released an Advisory on Social Media and Youth Mental Health, calling for swift, multi-sector action to maximize the benefits and reduce the risk of harm posed by social media on the mental health of children and adolescents.61 Recognizing these risks, NIMH is supporting research on understanding bidirectional relationships between social media use and adolescent mental health, psychiatric symptoms, and risk or resilience for psychopathology.62,63 For example, NIMH-funded researchers are investigating several critical areas, including relationships between social media use and disorders such as anxiety64,65 and disordered eating,66 effects of early smartphone use,67,68 and social media use in minoritized youth.69,70 Despite the potential negative health outcomes, social media may still be a useful tool that can identify youth at risk and as an intervention tool to improve health. Looking forward, there is a need to identify risk and protective factors for technology and digital media use in youth that could inform potential targets for novel and improved interventions.
Biology of complex brain disorders. Collectively, mental and neurodevelopmental disorders exact a high toll in care and lost productivity in the United States. Recently, there has been substantial progress in accurately identifying common and rare disease-associated genetic variants that confer substantial risk for mental and neurodevelopmental disorders.71 Recognizing the opportunity this progress presents, NIMH is seeking to support research focused on probing brain biology at high resolution and sensitivity across different molecular, cellular, and circuit scales to identify the neural processes that may be differentially affected in complex brain disorders. Studies funded under this effort aim to incorporate molecular, cellular, and/or behavioral approaches to facilitate the characterization of intracellular, transcellular, and circuit mechanisms underlying complex brain function. This work will lead to a better understanding of the biology underlying risk for complex brain disorders and the context in which these risk factors act at molecular, cellular, and circuit levels. This work also will broadly benefit the study of genetic contributions to disease by increasing the accuracy and reliability of gene and protein network analyses for tissue- and cell-specific processes. Further, this effort aims to facilitate the identification of future targets of therapeutic intervention.
New pharmacological approaches. Effective pharmacological treatments exist for many mental illnesses; however, treatment-resistant mental illnesses remain a serious challenge. There is a need to improve existing treatments and develop new ones. NIMH aims to address this need by supporting research on pharmacological approaches that engage novel biological targets. As an example: for decades, most existing antidepressant medications have targeted the monoamine neurotransmitter system, but not all patients with depression respond to monoamine antidepressants. Years of NIMH-supported research led to the discovery that ketamine – a drug targeting the glutamate neurotransmitter system – has a robust, rapid therapeutic effect on treatment-resistant depression when administered intravenously.72 More recently, this line of research led to the development and FDA approval of the ketamine derivative, esketamine. Esketamine is effective for rapid relief of treatment-resistant depression, and can be administered more easily than ketamine, as a nasal spray.73
Psychedelic drugs such as psilocybin represent another area of active interest in the search for novel pharmacological approaches. Early clinical trial data suggest that these drugs may hold promise for treating depression and other mental and behavioral disorders.74 More research is needed to definitively establish their efficacy and long-term safety, and NIMH is actively engaging with the research community to fulfill this need.75 An important component of all of this work is NIMH’s sustained emphasis on the experimental therapeutics approach, in which studies not only determine the safety and effectiveness of therapeutics, but also generate knowledge about how the therapeutics engage their biological target.

Find an accessible version of the FY 2025 Budget Fact Sheet.
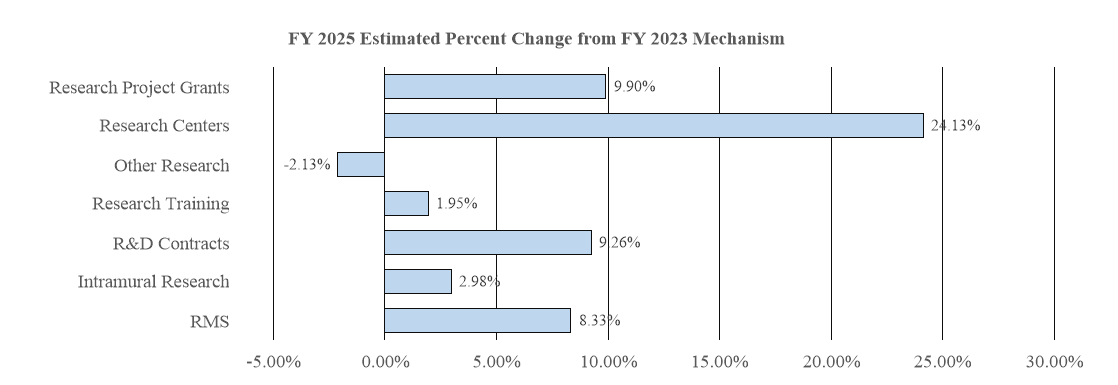
Major Changes
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanism and activity details and these highlights will not sum to the total change for the FY 2025 President’s Budget request for the National Institute of Mental Health (NIMH). The FY 2025 President’s Budget request is $2,548.7 million, an increase of $207.0 million compared to the FY 2023 Final level. The overall increase will help advance priorities such as the development of biomarkers and the development of methods to better predict patient prognosis and optimize treatment. The request includes $45.5 million in authorized funding provided through the 21st Century Cures Act for the Brain Research Through Advancing Innovative Neurotechnologies® (BRAIN) Initiative.
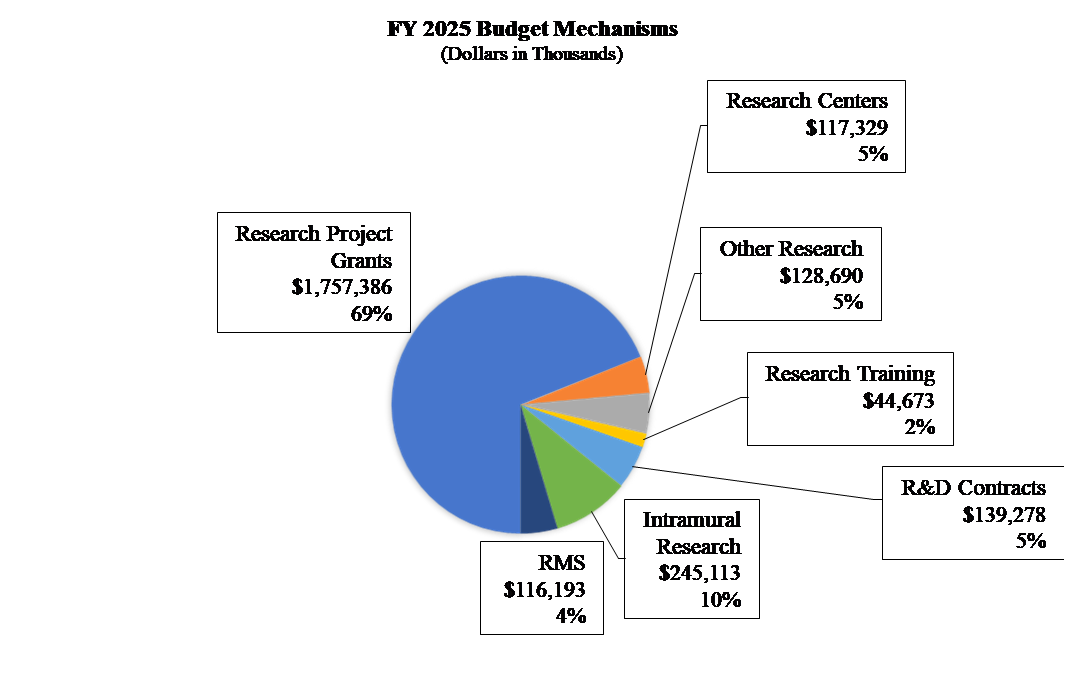
Research Project Grants (RPGs) (+$158.3 million; total $1,757.4 million)
NIMH expects to increase funding for non-competing RPGs by $57.7 million, to fund projects receiving competing awards in prior years. Competing RPGs are expected to increase by 239 grants or $96.9 million. This increase is distributed across all programmatic areas and basic, translational, or clinical research.
Research Centers (+$22.8 million; total $117.3 million)
NIMH expects to increase funding for Research Centers by $22.8 million to support additional ALACRITY Centers, Practice Based Suicide Prevention Research Centers, and additional Centers supporting therapeutic and service delivery interventions.
Other Research (-$2.8 million; total $128.7 million)
NIMH expects to decrease funding for Other Research by $2.8 million due to shifting funding from the Shared Instrumentation grants to other priorities.
Intramural Research Program (+$7.1 million; total $245.1 million)
NIMH expects to increase funding for Intramural Research by $7.1 million and will accelerate innovative research studies conducted by the Institute’s intramural scientists.
Research Management and Support (RMS) (+$8.9 million; total $116.2 million)
NIMH expects to increase funding for RMS by $8.9 million and will continue to support the oversight and management of scientific programs critical to fulfilling the Institute’s mission.
Budget Mechanism Table
| Mechanism | FY 2023 Final2 | FY 2024 CR | FY 2025 Presidents Budget | FY 2025 +/- FY 2023 | ||||
|---|---|---|---|---|---|---|---|---|
| Number | Amount | Number | Amount | Number | Amount | Number | Amount | |
| Research Projects: | ||||||||
| Noncompeting | 1,729 | $1,019,745 | 1,599 | $1,040,589 | 1,565 | $1,077,451 | -164 | $57,707 |
| Administrative Supplements | (165) | $22,120 | (136) | $18,492 | (136) | $18,540 | -(29) | -$3,580 |
| Competing: | ||||||||
| Renewal | 47 | $34,602 | 42 | $26,198 | 70 | $48,860 | 23 | $14,258 |
| New | 551 | $450,366 | 457 | $285,817 | 767 | $533,047 | 216 | $82,681 |
| Supplements | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Subtotal Competing | 598 | $484,969 | 499 | $312,015 | 837 | $581,907 | 239 | $96,939 |
| Subtotal RPGs | 2,327 | $1,526,833 | 2,098 | $1,371,095 | 2,402 | $1,677,898 | 75 | $151,065 |
| SBIR/STTR | 103 | $72,226 | 97 | $66,825 | 117 | $79,488 | 14 | $7,262 |
| Research Project Grants | 2,430 | $1,599,059 | 2,195 | $1,437,920 | 2,519 | $1,757,386 | 89 | $158,327 |
| Research Centers | ||||||||
| Specialized/Comprehensive | 40 | $94,523 | 45 | $108,095 | 45 | $117,329 | 5 | $22,805 |
| Clinical Research | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Biotechnology | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Comparative Medicine | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Research Centers in Minority Institutions | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Research Centers | 40 | $94,523 | 45 | $108,095 | 45 | $117,329 | 5 | $22,805 |
| Other Research | ||||||||
| Research Careers | 381 | $66,386 | 384 | $66,560 | 388 | $67,125 | 7 | $738 |
| Cancer Education | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Cooperative Clinical research | 0 | $300 | 0 | $300 | 0 | $300 | 0 | $0 |
| Biomedical Research Support | 5 | $3,392 | 0 | $0 | 0 | $0 | -5 | -$3,392 |
| Minority Biomedical Research Support | 0 | $701 | 0 | $701 | 0 | $701 | 0 | $0 |
| Other | 72 | $60,718 | 64 | $62,691 | 64 | $60,565 | -8 | -$153 |
| Other Research | 458 | $131,497 | 448 | $130,252 | 452 | $128,690 | -6 | -$2,807 |
| Total Research Grants | 2,928 | $1,825,080 | 2,688 | $1,676,267 | 3,016 | $2,003,405 | 88 | $178,325 |
| Ruth L. Kirschstein Training Awards | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 282 | $13,491 | 283 | $13,727 | 280 | $13,765 | -2 | $274 |
| Institutional Awards | 458 | $30,328 | 460 | $30,828 | 455 | $30,907 | -3 | $580 |
| Total Research Training | 740 | $43,819 | 743 | $44,555 | 735 | $44,673 | -5 | $854 |
| Research and Develop Contracts | 136 | $127,475 | 137 | $129,321 | 137 | $139,278 | 1 | $11,803 |
| (SBIR/STTR)(non-add) | (2) | ($783) | (0) | ($727) | 0 | ($713) | -($2) | -($70) |
| Intramural Research | 296 | $238,024 | 300 | $238,665 | 300 | $245,113 | 4 | $7,090 |
| Res. Management and Support | 309 | $107,256 | 323 | $110,035 | 335 | $116,193 | 26 | $8,937 |
| (SBIR Admin) (non-add) | ($6) | ($150) | ($150) | ($144) | ||||
| Construction | $0 | $0 | $0 | $0 | ||||
| Buildings and Facilities | $0 | $0 | $0 | $0 | ||||
| Total NIMH | 605 | $2,341,653 | 623 | $2,198,843 | 635 | $2,548,662 | 30 | $207,009 |
* All items in italics and brackets are non-add entries.
1 Of which $225.0 million in FY 2023, $86.0 million in FY 2024 and $45.5 million in FY 2025 is derived by transfer from the NIH Innovation Account under the 21st Century Cures Act.
2 Includes FY 2023 21st Century Cures Act funding not obligated in FY 2023 and carried into FY 2024.
Appropriations Language
NATIONAL INSTITUTES OF HEALTH
NATIONAL INSTITUTE OF MENTAL HEALTH
For carrying out section 301 and title IV of the PHS Act with respect to mental health, $2,503,162,000.
NIH INNOVATION ACCOUNT, CURES ACT
(INCLUDING TRANSFER OF FUNDS)
For necessary expenses to carry out the purposes described in section 1001(b)(4) of the 21st Century Cures Act, in addition to amounts available for such purposes in the appropriations provided to the NIH in this Act, $127,000,000, to remain available until expended: Provided, That such amounts are appropriated pursuant to section 1001(b)(3) of such Act, are to be derived from amounts transferred under section 1001(b)(2)(A) of such Act, and may be transferred by the Director of the National Institutes of Health to other accounts of the National Institutes of Health solely for the purposes provided in such Act: Provided further, That upon a determination by the Director that funds transferred pursuant to the previous proviso are not necessary for the purposes provided, such amounts may be transferred back to the Account: Provided further, That the transfer authority provided under this heading is in addition to any other transfer authority provided by law.
[Top]
Summary of Changes
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
Summary of Changes
(Dollars in Thousands)
| CHANGES | FY 2023 Final | FY 2025 President's Budget | Built in change from FY 2023 Final | |||
|---|---|---|---|---|---|---|
| FTE's | Budget Authority | FTE's | Budget Authority | FTE's | Budget Authority | |
| 1. Intramural Research: | ||||||
| A. Built-in cost changes | ||||||
| a. FY 2024 effect of FY 2023 pay & benefits increase | $81,360 | $89,271 | $959 | |||
| b. FY 2024 effect of FY 2024 pay & benefits increase | $81,360 | $89,271 | $3,166 | |||
| c. FY 2024 Paid days adjustment | $81,360 | $89,271 | $313 | |||
| d. Differences attributable to FY 2024 change in FTE | $81,360 | $89,271 | $1,118 | |||
| e. FY 2025 effect of FY 2024 pay & benefits increase | $81,360 | $89,271 | $1.087 | |||
| f. FY 2025 effect of FY 2025 pay & benefits increase | $81,360 | $89,271 | $1,452 | |||
| g. FY 2025 Paid days adjustment | $81,360 | $89,271 | $0 | |||
| h. Differences attributable to FY 2025 change in FTE | $81,360 | $89,271 | $0 | |||
| i. Payment for centrally furnished services | $37,195 | $39,882 | $2,687 | |||
| j. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | $119,469 | $115,960 | $9,041 | |||
| Subtotal, IR built-in cost changes | $19,824 | |||||
| 2. Research Management and Support: | ||||||
| A. Built-in cost changes | ||||||
| a. FY 2024 effect of FY 2023 pay & benefits increase | $54,470 | $63,791 | $644 | |||
| b. FY 2024 effect of FY 2024 pay & benefits increase | $54,470 | $63,791 | $2,119 | |||
| c. FY 2024 Paid days adjustment | $54,470 | $63,791 | $210 | |||
| d. Differences attributable to FY 2024 change in FTE | $54,470 | $63,791 | $2,576 | |||
| e. FY 2025 effect of FY 2024 pay & benefits increase | $54,470 | $63,791 | $747 | |||
| f. FY 2025 effect of FY 2025 pay & benefits increase | $54,470 | $63,791 | $1,015 | |||
| g. FY 2025 Paid days adjustment | $54,470 | $63,791 | $0 | |||
| h. Differences attributable to FY 2025 change in FTE | $54,470 | $63,791 | $2,318 | |||
| i. Payment for centrally furnished services | $7,346 | $7,877 | $531 | |||
| j. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | $45,430 | $44,525 | $3,031 | |||
| Subtotal, RMS built-in cost changes | $13,191 | |||||
| FY 2023 Final | FY 2025 President's Budget | Program change from FY 2023 Final | ||||
| Changes | No. | Amount | No. | Amount | No. | Amount |
| B. Program: | ||||||
| 1. Research Project Grants: | ||||||
| a. Noncompeting | 1,729 | $1,041,864 | 1,565 | $1,095,991 | -164 | $54,126 |
| b. Competing | 598 | $484,969 | 837 | $581,907 | 239 | $96,939 |
| c. SBIR/STTR | 103 | $72,226 | 117 | $79,488 | 14 | $7,262 |
| Subtotal, RPGs | 2,430 | $1,599,059 | 2,519 | $1,757,386 | 89 | $158,327 |
| 2. Research Centers | 40 | $94,523 | 45 | $117,329 | 5 | $22,805 |
| 3. Other Research | 458 | $131,497 | 452 | $128,690 | -6 | -$2,807 |
| 4. Research Training | 740 | $43,819 | 735 | $44,673 | -5 | $854 |
| 5. Research and development contracts | 136 | $127,475 | 137 | $139,278 | 1 | $11,803 |
| Subtotal, Extramural | $1,996,374 | $2,187,356 | $190,982 | |||
| FTEs | FTEs | FTEs | ||||
| 6. Intramural Research | 296 | $238,024 | 300 | $245,113 | 4 | -$12,734 |
| 7. Research Management and Support | 309 | $107,256 | 335 | $116,193 | 26 | -$4,254 |
| 8. Construction | $0 | $0 | $0 | |||
| 9. Buildings and Facilities | $0 | $0 | $0 | |||
| Subtotal, program changes | $173,994 | |||||
| Total built-in and program changes | 605 | $2,341,653 | 635 | $2,548,662 | 30 | $207,009 |
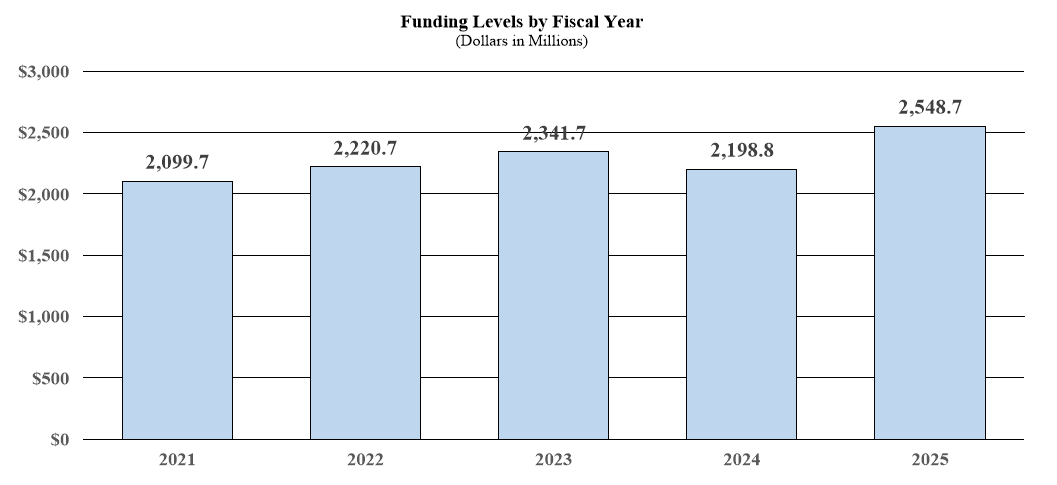
Budget Graphs
History of Budget Authority and FTEs:
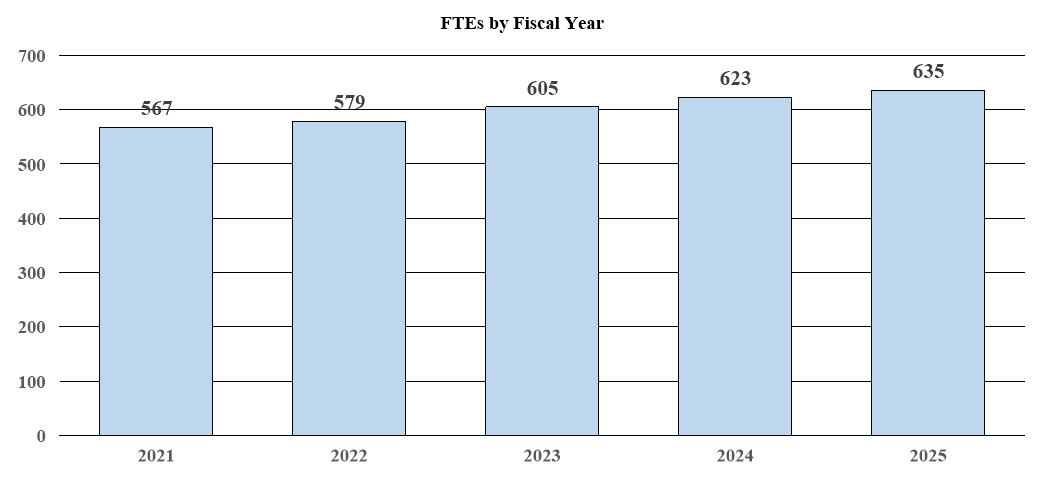
Distribution by Mechanism:
Change by Selected Mechanism:
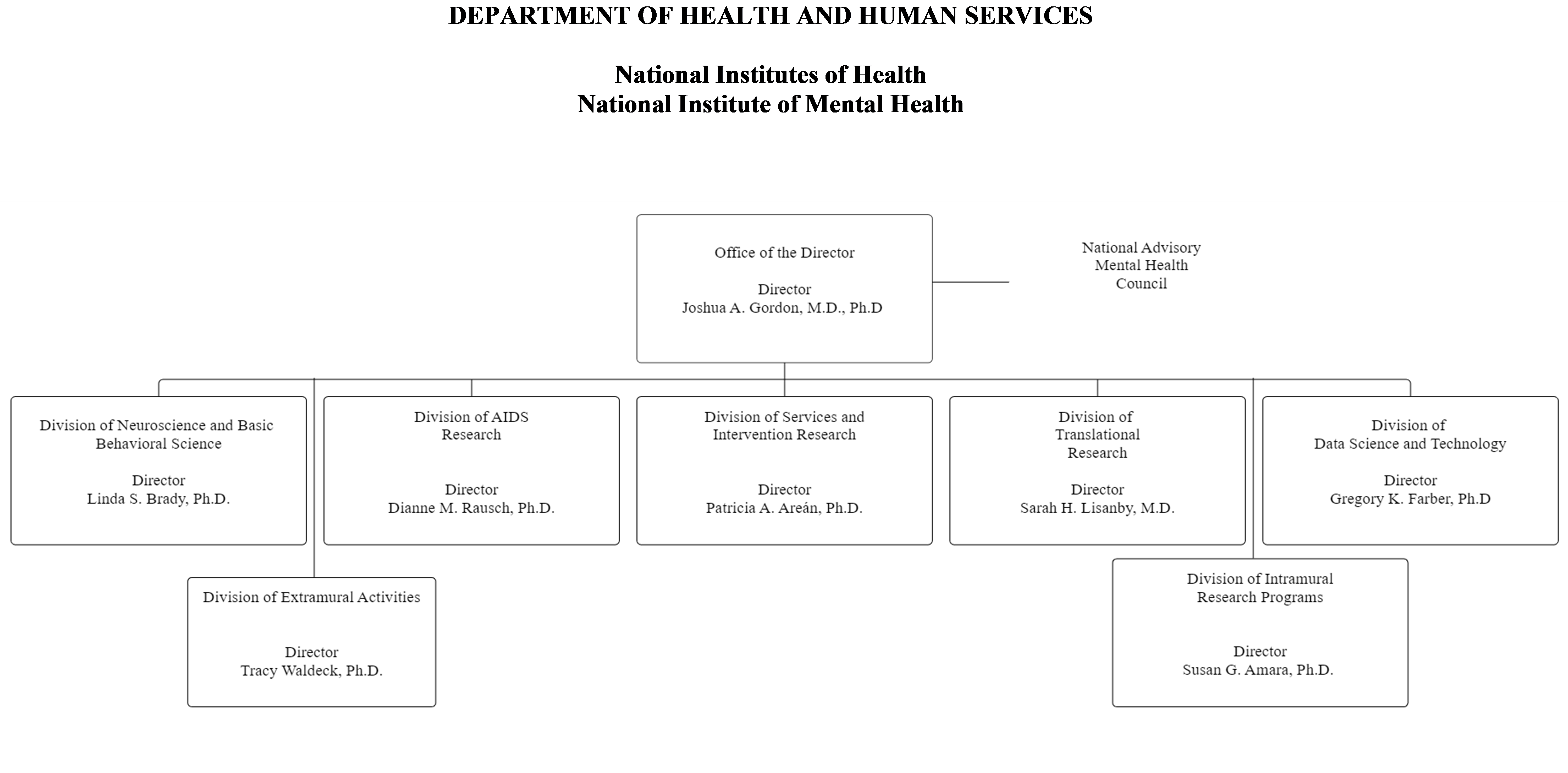
Organization Chart
National Institutes of Health
National Institute of Mental Health
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
Budget Authority by Activity
| Extramural Research | FY 2023 Final | FY 2024 CR | FY 2025 President's Budget | FY 2025 +/- FY 2023 Final | ||||
|---|---|---|---|---|---|---|---|---|
| FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount | |
| Detail | ||||||||
| Neuroscience & Basic Behavioral Science | $719,354 | $662,663 | $795,375 | $76,021 | ||||
| Services & Intervention Research | $261,840 | $241,205 | $289,511 | $27,671 | ||||
| Translational Research | $589,372 | $542,925 | $651,656 | $62,284 | ||||
| Data Science & Technology | $216,907 | $199,813 | $239,829 | $22,923 | ||||
| AIDS Research | $189,191 | $185,381 | $189,191 | $0 | ||||
| Office of the Director | $19,710 | $18,157 | $21,793 | $2,083 | ||||
| Subtotal, Extramural | $1,996,374 | $1,850,143 | $2,187,356 | $190,982 | ||||
| Intramural Research | 296 | $238,024 | 300 | $238,665 | 300 | $245,113 | 4 | $7,090 |
| Research Management & Support | 309 | $107,256 | 323 | $110,035 | 335 | $116,193 | 26 | $8,937 |
| Total | 605 | $2,341,653 | 623 | $2,198,843 | 635 | $2,548,662 | 30 | $207,009 |
*Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
Justification of Budget Request
National Institute of Mental Health
Authorizing Legislation: Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA): [placeholder table]
| FY 2023 Final | FY 2024 CR | FY 2025 President’s Budget | FY 2025 +/- FY 2023 | |
| BA | $2,341,653,000 | $2,198,843,000 | $2,548,662,000 | $207,009,000 |
| FTE | 605 | 623 | 635 | +30 |
[Top]
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
Overall Budget Policy: The FY 2025 President’s Budget request for the National Institute of Mental Health (NIMH) is $2,548.7 million, an increase of $207.0 million or 8.8 percent compared to the FY 2023 Final. The request includes $10.0 million for a behavioral health science implementation initiative and $190.0 million for other mental health research supporting better diagnostics, improved treatments, and enhanced precision of mental health care. The request also includes 21st Century Cures Act authorized funding of $45.5 million for the Brain Research Through Advancing Innovative Neurotechnologies (BRAIN)® Initiative, which is a reduction of $179.5 million from the authorized level in FY 2023. To offset this decrease, the request includes an increase of $179.5 million in non-Cures Act funding for the BRAIN Initiative to maintain the total FY 2023 Enacted level for the program.
Program Descriptions
Office of the Director
The NIMH Office of the Director (OD) leads the institute in carrying out the NIMH mission to transform the understanding and treatment of mental illnesses. The OD provides scientific leadership, sets programmatic priorities, coordinates cross-cutting programs, determines institute policies, directly funds several research projects, and provides overall administrative and operational coordination for the institute. The OD houses eight offices: Office on AIDS; Office of National Autism Coordination; Office of Clinical Research; Office of Genomics Research Coordination; Office for Disparities Research and Workforce Diversity; Office of Management; Office of Rural Mental Health Research; and Office of Science Policy, Planning, and Communications. Each of the offices within the OD play an important role in supporting the institute.
As an example of research that the OD prioritizes, NIMH is supporting research to better understand factors that confer risk and resilience for suicide among Black youth,76 whose rates of death by suicide have risen at an alarming rate in recent years.77 Understanding how social determinants of health interact with biological and behavioral risk and protective factors is a necessary step in identifying underlying mechanisms that can inform the development of effective suicide prevention strategies for Black youth. In alignment with the National Action Alliance for Suicide Prevention, NIMH continues to pursue the goal of reducing the rate of suicide in the United States by 20 percent by the year 2025.78 Suicide is the second leading cause of death for youth aged 10-24 years, and certain subgroups of youth are at significantly elevated risk, so focusing research efforts on high-risk youth is critical to achieving this goal. Similarly, NIMH is supporting research to better understand risk and resilience for mental illnesses in Asian American, Native Hawaiian, and Pacific Islander subpopulations.79 Additionally, the OD supports research on neuroethics through the BRAIN Initiative.
Budget Policy: The FY 2025 President’s Budget request is $21.8 million, an increase of $2.1 million or 10.6 percent compared with the FY 2023 Final.
Neuroscience and Basic Behavioral Science
The Division of Neuroscience and Basic Behavioral Science (DNBBS) supports research in the areas of basic molecular and cellular neuroscience, genetics, integrative neuroscience, research training, and drug discovery. In collaboration with other NIMH programs and the wider research community, the Division ensures that relevant basic scientific knowledge is generated and used in pursuit of improved methods that, in the long term, could be used to diagnose, treat, and prevent mental illnesses.
DNBBS funds grants across a range of research topics to enhance understanding of the basic neurobiology underlying mental illnesses. In FY 2024, DNBBS is continuing efforts to develop measures of brain activity in animals that aim to provide insights into the discovery and development of novel mechanisms for the treatment of mental disorders. In addition, DNBBS is expanding a broad, coordinated effort to understand how genetic alterations found in psychiatric patients act in brain cells to cause changes in cellular and circuit function, and ultimately behavior. Through the BRAIN Initiative, DNBBS also supports research focused on characterizing brain cell types and developing human cell-based models for studying the brain.
Budget Policy: The FY 2025 President’s Budget request is $795.4 million, an increase of $76.0 million or 10.6 percent compared with the FY 2023 Final.
Program Portrait – Accelerating Medicines Partnership® Program - Schizophrenia (AMP® SCZ).
In September 2020, in collaboration with the Foundation for the National Institutes of Health, the Food and Drug Administration, and multiple public and private partners, NIMH launched the Accelerating Medicines Partnership® Schizophrenia (AMP SCZ) initiative.80 Part of the broader NIH AMP program, AMP SCZ aims to develop tools that identify the early stages of risk for schizophrenia and predict the likelihood of progression to psychosis and other outcomes.81 A related AMP SCZ aim is to develop tools that can help researchers identify new targets for drug-based treatments that can be tested in clinical trials. The initiative has established a Research Network and a Data Processing, Analysis, and Coordinating Center to allow researchers to integrate and analyze data from the NIMH Data Archive.82 NIMH expects to contribute $99.4 million over five years and is currently supporting three AMP SCZ research projects.83,84,85 Findings from these studies may enable researchers to develop predictive algorithms for the course of illness, allowing for early interventions that may prevent the development of schizophrenia and improve a person’s clinical and functional outcomes. In June 2022, researchers involved in the AMP SCZ program began enrolling research study participants. Forty-three recruitment sites across North and South America, Europe, Asia, and Australia aim to enroll 1,977 people at clinical high risk for psychosis and 640 healthy controls, between the age of 12-30. AMP SCZ investigators have also reported on the development of a harmonized clinical outcome assessment instrument.86
Translational Research
The Division of Translational Research (DTR) supports integrative, multidisciplinary research and training programs that translate findings from basic science to discover the causes, mechanisms, and trajectories of mental illnesses, and to develop effective interventions for individuals across the lifespan. DTR supports research using innovative forms of scientific analysis, including computational psychiatry and machine learning, to elucidate the characteristics of, and risk factors for, mental illnesses; the neurobehavioral mechanisms of psychopathology; the trajectories of risk and resilience based on the interactive influences of genetics, brain development, environment, and experience; and the design and testing of innovative treatments and interventions. DTR-supported research efforts may have intermediate-term impact and pave the way towards safe and effective treatment for and prevention of mental illnesses. One area of high priority for DTR is to fund research to improve outcomes for individuals at clinical high risk (CHR) for psychosis. A major knowledge gap has been the lack of a means to reliably predict which individuals with CHR will develop schizophrenia or other adverse outcomes. Such knowledge could enable the implementation of effective prevention strategies. To address this gap, the major public-private partnership AMP® SCZ87 seeks to prevent the development of schizophrenia and other outcomes of CHR associated with significant disability (see “Program Portrait – Accelerating Medicines Partnership® Program - Schizophrenia (AMP® SCZ)”). This flagship study builds on the successes of prior investments to identify biomarkers of risk for progression to schizophrenia, including the North American Prodrome Longitudinal Study (NAPLS) which identified promising biomarkers of risk102,103 and developed a risk calculator to predict conversion to psychosis.104
In addition, DTR, in collaboration with the Department of Defense, private foundations, and industry, supports the Advancing Understanding of RecOvery afteR traumA (AURORA) Study,105 a landmark study to understand the consequences of trauma, as well as research using advanced digital techniques, including natural language processing,106 machine learning, and predictive coding,107 that aim to predict mental health outcomes, such as risk for suicide. DTR also supports work harnessing the latest advances in artificial intelligence to advance mechanistic understanding of how circuits in the brain shape behavior.108
Budget Policy: The FY 2025 President’s Budget request is $651.7 million, an increase of $62.3 million or 10.6 percent compared with the FY 2023 Final.
Program Portrait – Understanding Suicide Risk and Protective Factors among Black Youth.
Suicide rates among Black youth nearly doubled between 1999 and 2018, and Black youth under 13 years of age are approximately twice as likely to die by suicide as their white counterparts.88,89 NIMH is supporting research to understand systems-level risk detection and interventions that can reduce self-harm and suicidal thoughts and behaviors in Black children and adolescents,90,91 as well as studies of school-based suicide prevention programs for Black youth.92,93,94 Additionally, NIMH recently solicited research aimed at better characterizing risk trajectories and protective factors among Black youth.95,96 In one recently funded study, researchers are testing whether experiences like loneliness, low self-worth, and hopelessness early in childhood are linked to risk for suicide, and whether protective factors such as racial socialization and racial identity protect Black youth from developing suicidal thoughts.97 Other recently funded projects focus on intersectional approaches to suicide prevention tailored for Black youth who are sexual and gender minorities or have been involved in the juvenile justice system.98,99 NIMH is also soliciting research to better identify and measure suicide risk and protective factors among preteens (ages 8-12), including Black youth and those who may experience health disparities or are underrepresented in research.100,101
Services and Intervention Research
The Division of Services and Intervention Research (DSIR) supports research that evaluates the effectiveness of psychosocial, pharmacological, somatic, rehabilitative, and combined interventions to prevent or treat mental illnesses and adverse consequences of mental illnesses (e.g., suicide, functional disability, lost productivity). DSIR funds research to refine and evaluate interventions for children, adolescents, adults and people who are underserved by mental health/behavioral health resources, focusing on acute and long-term symptom reduction, remission, and improved community functioning. DSIR also supports mental health services research to improve the quality and outcomes of care; organization- and system-level interventions to enhance service delivery to increase mental health equity and parity; and strategies for widespread dissemination and implementation of evidence-based treatments into routine care settings in all geographic areas (rural, urban, frontier, and island) and communities
DSIR initiatives encourage practice-based research with near-term potential for improving intervention effectiveness and service delivery, as illustrated by key research programs. For example, the Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness (ALACRITY) Research Centers aim to advance clinical practice and generate knowledge that will fuel the transformation of mental health care in the United States.110 A related program supports Practice-Based Suicide Prevention Research Centers that address NIMH suicide prevention research priorities and goals to reduce the national suicide rate.111,112
Budget Policy: The FY 2025 President’s Budget request is $289.5 million, an increase of $27.7 million or 10.6 percent compared with the FY 2023 Final.
Program Portrait – SSPsyGene: Scalable and Systematic Neurobiology of Psychiatric and Neurodevelopmental Disorder Risk Genes: Data Resource and Administrative Coordination Center.
Despite accelerated discovery of disease genes over the past decade, we have limited understanding of how genes impact the development and occurrence of mental disorders. NIMH’s Scalable and Systematic Neurobiology of Psychiatric and Neurodevelopmental Disorder Risk Genes (SSPsyGene) Consortium aims to comprehensively characterize the function of genes in the brain in which variants increase risk for neurodevelopmental and psychiatric disorders.109 Through this initiative, NIMH is establishing a consortium of investigators at multiple sites and with broad expertise in the areas of genomics and neurobiology. In the first phase of the initiative, researchers plan to use scalable experimental systems with high-throughput capabilities to examine the biological function of 100-250 genes linked to neurodevelopmental and psychiatric disorders such as intellectual disability, autism spectrum disorder, and schizophrenia. As opposed to current small-scale efforts, SSPsyGene may provide a collaborative and efficient framework to identify genes’ biological function and generate a standardized, functional catalog of risk genes that may improve current approaches to diagnose, treat, and prevent mental disorders.
Division of Data Science and Technology
The Division of Data Science and Technology (DST) supports basic and applied research focused on the development of scientific tools, technologies, and approaches related to brain and behavioral research, including software (e.g., neuroinformatics tools and resources), hardware (e.g., devices and instrumentation), and wetware (e.g., novel genetic methods or bioactive and molecular imaging agents). DST functions include coordinating NIMH efforts and initiatives focused on advancing technology development and scientific informatics. DST also manages a variety of infrastructure programs for mental health researchers such as the NIMH Data Archive,113 the Brain Research Through Advancing Innovative Neurotechnologies® (BRAIN) Initiative data archives,114 the shared instrument program, the NeuroBioBank,115 and non-human primate colonies.
Budget Policy: The FY 2025 President’s Budget request is $239.8 million, an increase of $22.9 million or 10.6 percent compared with the FY 2023 Final.
AIDS Research
The Division of AIDS Research (DAR) supports research and research training that addresses the priority areas outlined in the NIH Strategic Plan for HIV and HIV-Related Research116 and the HHS National HIV/AIDS Strategy.117 DAR-supported research includes behavioral, social, data, and communications science studies aimed at reducing HIV/AIDS incidence through the development, testing, and implementation of new and improved prevention strategies, and improving health outcomes and reducing health disparities of those living with HIV through improved linkage to care and adherence to effective treatments. DAR also supports research to better understand, prevent, and treat the neurological and mental disorders associated with HIV. DAR is participating in cure research by supporting studies to eradicate or silence HIV from biological reservoirs in the central nervous system (CNS), where the virus may evade detection and treatment. HIV latency in the CNS is critically important to consider in studies of eradication and reactivation. Many drugs designed to eradicate the virus are unable to penetrate the blood-brain barrier of the CNS, thus resulting in a protected reservoir of HIV. DAR places a strong emphasis on targeted research to understand the mechanisms underlying HIV-induced neuronal pathology and the resulting motor, cognitive, and psychiatric dysfunction that results, with the goal of identifying preventive and therapeutic interventions.
DAR-funded research also places special emphasis on World Health Organization-defined key populations, health disparities, and the impact of mental illnesses that may increase the risk for acquisition of HIV or negatively impact the health outcomes of those living with HIV. Additionally, DAR engages with multidisciplinary expertise in NIH-wide planning efforts to ensure effective integration of behavioral and biomedical approaches to help achieve an AIDS-free generation.
Budget Policy: The FY 2025 President’s Budget request is $189.2 million, sustaining the FY 2023 Final level.
Intramural Research Programs
The Division of Intramural Research Programs (IRP) is the internal research component of NIMH, complementing the institute’s extramural grant funding program. IRP scientists investigate basic, translational, and clinical aspects of brain function and behavior, conducting state-of-the-art research using unique NIH resources. In addition, the IRP provides an excellent environment for training the next generation of basic, translational, and clinical scientists.
IRP researchers are developing new and improved methods in functional magnetic resonance imaging118 (fMRI) and exploring advanced computational methods to evaluate brain function and mental illnesses. Many IRP researchers use neuroimaging, brain activity recording, and behavioral tasks to investigate differences in brain circuitry underlying key brain functions such as learning, perception, and attention, which are affected in mental illnesses. IRP researchers also use sophisticated experimental techniques such as optogenetic stimulation and two photon imaging to study brain function and behavior. For example, they demonstrated how the mammalian visual cortex can integrate and amplify direct excitatory input to drive a novel behavior, 119 or increase understanding of neuronal avalanches in the brain. 120,121 Understanding brain network dynamics and the circuit basis of adult learning might point towards targeted treatments to improve brain function.
IRP scientists are also exploring novel medications and other treatments for depression in adults, including ketamine and other experimental fast-acting antidepressant medications, next generation seizure therapy, and transcranial magnetic stimulation (TMS). Researchers are also using TMS to study auditory and language processing in adolescents with autism spectrum disorder. 122,123 Using clinical assessments, brain imaging, and sleep studies, researchers aim to better understand suicide.124 IRP researchers also continue to study youth suicide,125 including analysis of national suicide data during the COVID-19 pandemic.126,127
Budget Policy: The FY 2025 President’s Budget request is $245.1 million, an increase of $7.1 million or 3.0 percent compared with the FY 2023 Final.
Research Management and Support
Research Management and Support (RMS) activities provide administrative, budgetary, logistical, and scientific support in the review, award, and monitoring of research and training grants, and research and development contracts. RMS functions include strategic planning, coordination, and evaluation of NIMH programs, regulatory compliance, coordination of global mental health efforts, and liaising with other Federal agencies, Congress, and the public. Staff also play key roles in coordinating NIMH’s involvement in the NIH BRAIN Initiative and in managing related research. Through RMS activities, NIMH continues to provide accountability and administrative support for meritorious basic, clinical, and translational research and promote health information dissemination, education, and outreach activities. RMS also supports outreach activities to connect the public with evidence-based mental health information. For example, in recognition of National Suicide Prevention Awareness Month (September), NIMH promoted brochures, fact sheets, and graphics;128 highlighted the new 988 Suicide & Crisis Lifeline;129 and, co-hosted a Facebook Live event with the National Institute on Drugs and Addiction130 on the intersection of suicide and substance use.131 Information is presented in plain language and suitable for a lay audience, and many materials are available in Spanish to reach a broader audience.
Budget Policy: The FY 2025 President’s Budget request is $116.2 million, an increase of $8.9 million or 8.3 percent compared with the FY 2023 Final.
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation |
|---|---|---|---|---|
| 2016 | $1,489,417,000 | $1,512,401,000 | $1,520,260,000 | $1,548,390,000 |
| Rescission | $0 | |||
| 2017 1 | $1,518,673,000 | $1,599,747,000 | $1,619,537,000 | $1,601,931,000 |
| Rescission | $0 | |||
| 2018 2 | $1,244,901,000 | $1,668,461,000 | $1,724,568,000 | $1,754,775,000 |
| Rescission | $0 | |||
| 2019 2 | $1,612,192,000 | $1,790,231,000 | $1,871,250,000 | $1,870,296,000 |
| Rescission | $0 | |||
| 2020 2 | $1,630,422,000 | $1,961,704,000 | $2,076,244,000 | $2,038,374,000 |
| Rescission | $0 | |||
| 2021 2 | $1,844,865,000 | $2,060,303,000 | $2,139,491,000 | $2,103,708,000 |
| Rescission | $0 | |||
| 2022 2 | $2,213,574,000 | $2,223,085,000 | $2,218,900,000 | $2,216,976,000 |
| Rescission | $0 | |||
| 2023 2 | $2,210,828,000 | $2,428,775,000 | $2,332,672,000 | $2,337,843,000 |
| Rescission | $0 | |||
| 2024 2 | $2,541,653,000 | $2,198,843,000 | $2,437,843,000 | $2,198,843,000 |
| 2025 | $2,548,662,000 |
1 Budget Estimate to Congress includes mandatory financing.
2 Includes funds derived by transfer from the NIH Innovation Account under the 21st Century Cures Act
[Top]
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2024 Amount Authorized | FY 2024 CR | 2025 Amount Authorized | FY 2025 President’s Budget | |
| Research and Investigation | Section 301 | 42§241 | Indefinite | $2,198,843,000 | Indefinite | $2,548,662,000 |
| National Institute of Mental Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||
| Total Budget Authority | $2,198,843,000 | $2,548,662,000 |
[Top]
Amounts Available for Obligation
| Source of Funding | FY 2023 Final | FY 2024 CR | FY 2025 President's Budget |
| Appropriation2 | $2,337,843 | $2,198,843 | $2,548,662 |
| Mandatory Appropriation: (non-add) | |||
| Type 1 Diabetes | ($0) | ($0) | ($0) |
| Other Mandatory financing | ($0) | ($0) | ($0) |
| Subtotal, adjusted appropriation | $2,337,843 | $2,198,843 | $2,548,662 |
| OAR HIV/AIDS Transfers | $3,810 | $0 | $0 |
| Subtotal, adjusted budget authority | $2,341,653 | $2,198,843 | $2,548,662 |
| Unobligated balance, start of year | $10,270 | $84,980 | $0 |
| Unobligated balance, end of year (carryover)3 | -$84,980 | $0 | $0 |
| Subtotal, adjusted budget authority | $2,266,943 | $2,283,823 | $2,548,662 |
| Unobligated balance lapsing | -$10 | $0 | $0 |
| Total obligations | $2,266,933 | $2,283,923 | $2,548,662 |
1 Excludes the following amounts (in thousands) for reimbursable activities carried out by this account: FY 2023 - $8,014 FY 2024 - $10,050 FY 2025 - $10,050
2 Of which $225.0 million in FY 2023, $86.0 million in FY 2024, and $45.5 million in FY 2025 is derived by transfer from the NIH InnovationAccount under the 21st Center Cures Act
3 Includes 21st Century Cures Act funding not obligated in FY 2023 and carried into 2024
[Top]
Budget Authority by Object Class
(Dollars in Thousands)
| FY 2024 CR | FY 2025 President's Budget | |
| Total compensable workyears: | ||
| Full-time equivalent | 623 | 635 |
| Full-time equivalent of overtime and holiday hours | 0 | 0 |
| Average ES salary | $223 | $228 |
| Average GM/GS grade | 12.9 | 12.9 |
| Average GM/GS salary | $141 | $145 |
| Average salary, Commissioned Corps (42 U.S.C. 207) | $0 | $0 |
| Average salary of ungraded positions | $163 | $168 |
| OBJECT CLASSES | FY 2024 CR | FY 2025 President's Budget |
| Personnel Compensation | ||
| 11.1 Full-Time Permanent | $60,707 | $63,956 |
| 11.3 Other Than Full-Time Permanent | $30,116 | $30,960 |
| 11.5 Other Personnel Compensation | $3,590 | $3,691 |
| 11.7 Military Personnel | $0 | $0 |
| 11.8 Special Personnel Services Payments | $16,691 | $17,159 |
| 11.9 Subtotal Personnel Compensation | $111,105 | $115,765 |
| 12.1 Civilian Personnel Benefits | $35,512 | $37,297 |
| 12.2 Military Personnel Benefits | $0 | $0 |
| 13.0 Benefits to Former Personnel | $0 | $0 |
| Subtotal Pay Costs | $146,617 | $153,062 |
| 21.0 Travel & Transportation of Persons | $2,809 | $2,871 |
| 22.0 Transportation of Things | $356 | $364 |
| 23.1 Rental Payments to GSA | $0 | $0 |
| 23.2 Rental Payments to Others | $0 | $0 |
| 23.3 Communications, Utilities & Misc. Charges | $1,387 | $1,417 |
| 24.0 Printing & Reproduction | $0 | $0 |
| 25.1 Consulting Services | $112,074 | $114,622 |
| 25.2 Other Services | $47,094 | $48,130 |
| 25.3 Purchase of Goods and Services from Government Accounts | $138,297 | $150,089 |
| 25.4 Operation & Maintenance of Facilities | $280 | $282 |
| 25.5 R&D Contracts | $11,304 | $11,553 |
| 25.6 Medical Care | $55 | $57 |
| 25.7 Operation & Maintenance of Equipment | $6,057 | $6,190 |
| 25.8 Subsistence & Support of Persons | $0 | $0 |
| 25.0 Subtotal Other Contractual Services | $315,162 | $330,922 |
| 26.0 Supplies & Materials | $5,155 | $5,269 |
| 31.0 Equipment | $5,516 | $5,637 |
| 32.0 Land and Structures | $1,014 | $1,036 |
| 33.0 Investments & Loans | $0 | $0 |
| 41.0 Grants, Subsidies and Contributions | $1,720,821 | $2,048,078 |
| 42.0 Insurance Claims and Indemnities | $0 | $0 |
| 43.0 Interest & Dividends | $6 | $6 |
| 44.0 Refunds | $0 | $0 |
| Subtotal Non-Pay Costs | $2,052,226 | $2,395,600 |
| Total Budget Authority by Object Class | $2,198,843 | $2,548,662 |
1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
[Top]
Salaries and Expenses
(Dollars in Thousands)
| OBJECT CLASSES | FY 2024 CR | FY 2025 President's Budget |
| Personnel Compensation | ||
| Full-Time Permanent (11.1) | $60,707 | $63,956 |
| Other Than Full-Time Permanent (11.3) | $30,116 | $30,960 |
| Other Personnel Compensation (11.5) | $3,590 | $3,691 |
| Military Personnel (11.7) | $0 | $0 |
| Special Personnel Services Payments (11.8) | $16,691 | $17,159 |
| Subtotal Personnel Compensation (11.9) | $111,105 | $115,765 |
| Civilian Personnel Benefits (12.1) | $35,512 | $37,297 |
| Military Personnel Benefits (12.2) | $0 | $0 |
| Benefits to Former Personnel (13.0) | $0 | $0 |
| Subtotal Pay Costs | $146,617 | $153,602 |
| Travel & Transportation of Persons (21.0) | $2,809 | $2,871 |
| Transportation of Things (22.0) | $356 | $364 |
| Rental Payments to Others (23.2) | $0 | $0 |
| Communications, Utilities & Misc. Charges (23.3) | $1,387 | $1,417 |
| Printing & Reproduction (24.0) | $0 | $0 |
| Other Contractual Services: | ||
| Consultant Services (25.1) | $58,681 | $60,480 |
| Other Services (25.2) | $47,094 | $48,310 |
| Purchase of Goods and Services from Government Accounts (25.3) | $79,148 | $81,139 |
| Operation & Maintenance of Facilities (25.4) | $280 | $282 |
| Operation & Maintenance of Equipment (25.7) | $6,057 | $6,190 |
| Subsistence & Support of Persons (25.8) | $0 | $0 |
| Subtotal Other Contractual Services | $191,260 | $196,220 |
| Supplies & Materials (26.0) | $5,155 | $5,269 |
| Subtotal Non-Pay Costs | $200,967 | $206,141 |
| Total Administrative Costs | $347,584 | $359,203 |
[Top]
Detail of Full-Time Equivalent Employment (FTE)
| Office/Division | FY 2023 Final | FY 2024 CR | FY 2025 President's Budget | ||||||
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of Extramural Activities | |||||||||
| Direct: | 45 | - | 45 | 47 | - | 47 | 49 | - | 49 |
| Total: | 45 | - | 45 | 47 | - | 47 | 49 | - | 49 |
| Division of Translational Research | |||||||||
| Direct: | 34 | - | 34 | 36 | - | 36 | 38 | - | 38 |
| Total: | 34 | - | 34 | 36 | - | 36 | 38 | - | 38 |
| Office of the Director | |||||||||
| Direct: | 141 | - | 141 | 146 | - | 146 | 148 | - | 148 |
| Reimbursable: | 13 | - | 13 | 13 | - | 13 | 13 | - | 13 |
| Total: | 154 | - | 154 | 159 | - | 159 | 161 | - | 161 |
| Division of Neuroscience and Basic Behavioral Science | |||||||||
| Direct: | 31 | - | 31 | 33 | - | 33 | 35 | - | 35 |
| Total: | 31 | - | 31 | 33 | - | 33 | 35 | - | 35 |
| Division of AIDS Research | |||||||||
| Direct: | 16 | - | 16 | 17 | - | 17 | 17 | - | 17 |
| Total: | 16 | - | 16 | 17 | - | 17 | 17 | - | 17 |
| Division of Services and Intervention Research | |||||||||
| Direct: | 15 | - | 15 | 16 | - | 16 | 18 | - | 18 |
| Total: | 15 | - | 15 | 16 | - | 16 | 18 | - | 18 |
| Data Science and Technology | |||||||||
| Direct: | 14 | - | 14 | 15 | - | 15 | 17 | - | 17 |
| Total: | 14 | - | 14 | 15 | - | 15 | 17 | - | 17 |
| Division of Intramural Research Programs | |||||||||
| Direct: | 291 | - | 291 | 295 | - | 295 | 295 | - | 295 |
| Reimbursable: | 5 | - | 5 | 5 | - | 5 | 5 | - | 5 |
| Total: | 296 | - | 296 | 300 | - | 300 | 300 | - | 300 |
| Total | 605 | - | 605 | 623 | - | 623 | 635 | - | 635 |
| Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
| FTE's supported by funds from Cooperative Research and Development Agreements | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fiscal Year | Average GS Grade |
| 2021 | 12.9 |
| 2022 | 13.0 |
| 2023 | 12.9 |
| 2024 | 12.9 |
| 2025 | 12.9 |
[Top]
Detail of Positions
| Grade | FY 2023 Final Final | FY 2024 CR | FY 2025 President's Budget |
|---|---|---|---|
| Total, ES Positions | 1 | 1 | 1 |
| Total, ES Salary | $212,100 | $222,811 | $227,880 |
| GM/GS-15 | 85 | 88 | 90 |
| GM/GS-14 | 89 | 92 | 94 |
| GM/GS-13 | 127 | 131 | 136 |
| GS-12 | 89 | 92 | 94 |
| GS-11 | 34 | 35 | 36 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 16 | 17 | 17 |
| GS-8 | 4 | 4 | 4 |
| GS-7 | 5 | 5 | 5 |
| GS-6 | 0 | 0 | 0 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 1 | 1 | 1 |
| GS-3 | 1 | 1 | 1 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 451 | 466 | 478 |
| Commissioned Corps (42 U.S.C. 207): | |||
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 0 | 0 | 0 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Junior Assistant | 0 | 0 | 0 |
| Subtotal | 0 | 0 | 0 |
| Ungraded | 180 | 180 | 180 |
| Total permanent positions | 451 | 466 | 478 |
| Total positions, end of year | 632 | 647 | 659 |
| Total full-time equivalent (FTE) employment, end of year | 605 | 623 | 635 |
| Average ES salary | $212,100 | $222,811 | $227,880 |
| Average GM/GS grade | 12.9 | 12.9 | 12.9 |
| Average GM/GS salary | $134,113 | $140,886 | $144,831 |
| 1Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||
References:
1 Substance Abuse and Mental Health Services Administration. (2022). Key substance use and mental health indicators in the United States: Results from the 2021 National Survey on Drug Use and Health (HHS Publication No. PEP22-07-01-005, NSDUH Series H-57). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from samhsa.gov/data/report/2021-nsduh-annual-national-report
2Institute of Health Metrics and Evaluation. ghdx.healthdata.org/gbd-results-tool accessed September 2023.
3cdc.gov/nchs/data/vsrr/vsrr034.pdf
4Centers for Disease Control and Prevention. (2022). Web-based Injury Statistics Query and Reporting System (WISQARS). Atlanta, GA: National Centers for Injury Prevention and Control, Centers for Disease Control and Prevention. Retrieved from cdc.gov/injury/wisqars/index.html
7nimh.nih.gov/about/strategic-planning-reports
8nimh.nih.gov/about/strategic-planning-reports/2022-strategic-plan-progress-report
9nimh.nih.gov/about/director/messages/2023/celebrating-nimhs-75-years
14pubmed.ncbi.nlm.nih.gov/37132201/
15reporter.nih.gov/project-details/10662398
16who.int/publications/i/item/9789241549790
17who.int/publications/i/item/9789240036703
18grants.nih.gov/grants/guide/rfa-files/RFA-MH-16-350.html
19grants.nih.gov/grants/guide/rfa-files/RFA-MH-23-260.html
20grants.nih.gov/grants/guide/rfa-files/RFA-MH-23-140.html
21grants.nih.gov/grants/guide/rfa-files/RFA-MH-23-310.html
22grants.nih.gov/grants/guide/rfa-files/RFA-MH-22-130.html
23grants.nih.gov/grants/guide/rfa-files/RFA-MH-23-300.html
24reporter.nih.gov/project-details/10417723
25pubmed.ncbi.nlm.nih.gov/28027368/
28grants.nih.gov/grants/guide/rfa-files/rfa-mh-19-150.html
29grants.nih.gov/grants/guide/rfa-files/RFA-MH-20-205.html
30grants.nih.gov/grants/guide/rfa-files/RFA-MH-19-151.html
32nationalepinet.org/core-assessment-battery-cab/
33cdc.gov/mmwr/volumes/72/wr/mm7206a4.htm?s_cid=mm7206a4_x
34Centers for Disease Control and Prevention. (2022). Web-based Injury Statistics Query and Reporting System (WISQARS). Atlanta, GA: National Centers for Injury Prevention and Control, Centers for Disease Control and Prevention. Retrieved from cdc.gov/injury/wisqars/index.html
35nimh.nih.gov/health/publications/nimh-strategic-framework-for-addressing-youth-mental-health
37reporter.nih.gov/project-details/10435003
38grants.nih.gov/grants/guide/rfa-files/RFA-MH-25-125.html
39grants.nih.gov/grants/guide/rfa-files/RFA-MH-25-126.html
40reporter.nih.gov/project-details/10440040
49nimh.nih.gov/health/topics/technology-and-the-future-of-mental-health-treatment
50grants.nih.gov/grants/guide/pa-files/PAR-23-096.html
51reporter.nih.gov/project-details/10462746
52grants.nih.gov/grants/guide/pa-files/PAR-20-243.html
53reporter.nih.gov/project-details/10362027
54reporter.nih.gov/project-details/10309487
55reporter.nih.gov/project-details/10593386
56reporter.nih.gov/project-details/10532198
57pubmed.ncbi.nlm.nih.gov/35277549/
58grants.nih.gov/grants/guide/rfa-files/RFA-MH-24-120.html
59grants.nih.gov/grants/guide/rfa-files/RFA-MH-23-105.html
60grants.nih.gov/grants/guide/rfa-files/RFA-MH-23-106.html
62grants.nih.gov/grants/guide/rfa-files/RFA-MH-23-115.html
63grants.nih.gov/grants/guide/rfa-files/RFA-MH-23-116.html
64reporter.nih.gov/project-details/10814547
65reporter.nih.gov/project-details/10815222
66reporter.nih.gov/project-details/10815182
67reporter.nih.gov/project-details/10813917
68reporter.nih.gov/project-details/10812927
69reporter.nih.gov/project-details/10815147
70reporter.nih.gov/project-details/10815348
71grants.nih.gov/grants/guide/pa-files/PAR-24-024.html
74pubmed.ncbi.nlm.nih.gov/33884324/
75nimh.nih.gov/news/events/2022/psychedelics-as-therapeutics-gaps-challenges-and-opportunities
76grants.nih.gov/grants/guide/rfa-files/RFA-MH-22-140.html
79grants.nih.gov/grants/guide/notice-files/NOT-MH-22-175.html
80nih.gov/research-training/accelerating-medicines-partnership-amp/schizophrenia
83reporter.nih.gov/project-details/10447770
84reporter.nih.gov/project-details/10440486
85reporter.nih.gov/project-details/10409839
86pubmed.ncbi.nlm.nih.gov/36640393/
89pubmed.ncbi.nlm.nih.gov/29799931/
90reporter.nih.gov/project-details/10440864
91reporter.nih.gov/project-details/10440599
92reporter.nih.gov/project-details/10338185
93reporter.nih.gov/project-details/10440929
94reporter.nih.gov/project-details/9807076
95grants.nih.gov/grants/guide/rfa-files/RFA-MH-22-140.html
96grants.nih.gov/grants/guide/rfa-files/RFA-MH-22-141.html
97reporter.nih.gov/project-details/10728686
98reporter.nih.gov/project-details/10729105
99reporter.nih.gov/project-details/10729187
100grants.nih.gov/grants/guide/rfa-files/RFA-MH-24-320.html
101grants.nih.gov/grants/guide/rfa-files/RFA-MH-24-322.html
102pubmed.ncbi.nlm.nih.gov/33667856/
103pubmed.ncbi.nlm.nih.gov/29971330/
104ncbi.nlm.nih.gov/pmc/articles/PMC5048498/
105reporter.nih.gov/project-details/10019595
106pubmed.ncbi.nlm.nih.gov/30710497/
107pubmed.ncbi.nlm.nih.gov/30389840/
108grants.nih.gov/grants/guide/pa-files/PAR-19-344.html
109grants.nih.gov/grants/guide/rfa-files/RFA-MH-22-110.html
111grants.nih.gov/grants/guide/pa-files/PAR-20-286.html
113nda.nih.gov/
114braininitiative.nih.gov/brain-programs/informatics
116oar.nih.gov/hiv-policy-and-research/strategic-plan
117hiv.gov/blog/hhs-and-the-national-hivaids-strategy
118pubmed.ncbi.nlm.nih.gov/37497043/
119pubmed.ncbi.nlm.nih.gov/37148876/
120pubmed.ncbi.nlm.nih.gov/37137888/
121nimh.nih.gov/news/science-news/2023/researchers-find-order-in-the-language-of-the-brain
122clinicaltrials.gov/study/NCT04798274
123decibels.ctss.nih.gov/index.html
124classic.clinicaltrials.gov/ct2/show/NCT02543983
125pubmed.ncbi.nlm.nih.gov/36789551/
126pubmed.ncbi.nlm.nih.gov/36789551/
127nimh.nih.gov/news/science-news/2023/youth-suicide-rates-increased-during-the-covid-19-pandemic
128nimh.nih.gov/get-involved/digital-shareables/shareable-resources-on-suicide-prevention
130The FY 2025 President’s Budget proposes to rename the National Institute on Drug Abuse to the National Institute on Drugs and Addiction.
131nimh.nih.gov/news/events/announcements/facebook-live-the-intersection-of-suicide-and-substance-use
