FY 2021 Budget - Congressional Justification
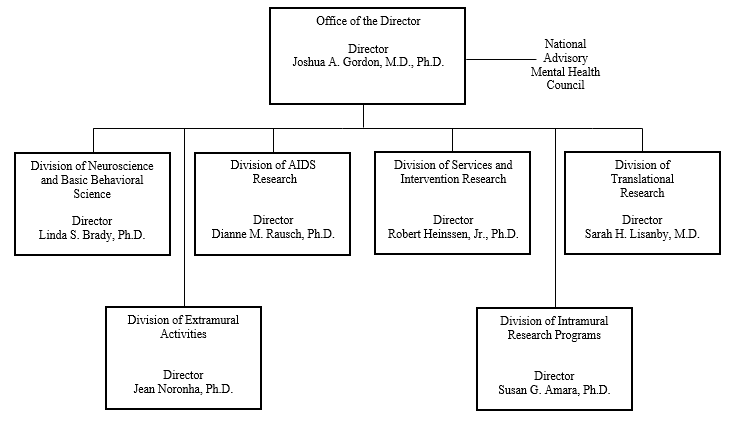
- Organization Chart
- Appropriation Language
- Amounts Available for Obligation
- Budget Mechanism Table
- Major Changes in Budget Request
- Summary of Changes
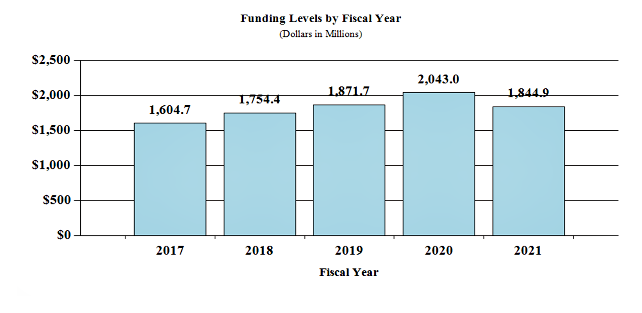
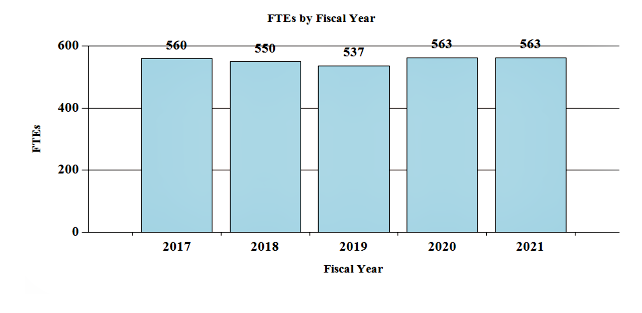
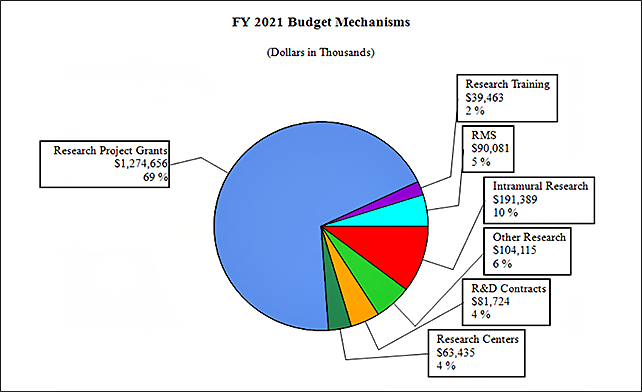
- Budget Graphs
- Budget Authority by Activity
- Authorizing Legislation
- Appropriations History
- Justification of Budget Request
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
Department of Health and Human Services
National Institutes of Health
National Institute of Mental Health
Organization Chart
[Top]
Appropriation Language
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
For carrying out section 301 and title IV of the PHS Act with respect to mental health, [$1,968,374,000]$1,794,865,000.
[Top]
NIH INNOVATION ACCOUNT, CURES ACT
(INCLUDING TRANSFER OF FUNDS)
For necessary expenses to carry out the purposes described in section 1001(b)(4) of the 21st Century Cures Act, in addition to amounts available for such purposes in the appropriations provided to the NIH in this Act, [$492,000,000]$404,000,000, to remain available until expended: Provided, That such amounts are appropriated pursuant to section 1001(b)(3) of such Act, are to be derived from amounts transferred under section 1001(b)(2)(A) of such Act, and may be transferred by the Director of the National Institutes of Health to other accounts of the National Institutes of Health solely for the purposes provided in such Act: Provided further, That upon a determination by the Director that funds transferred pursuant to the previous proviso are not necessary for the purposes provided, such amounts may be transferred back to the Account: Provided further, That the transfer authority provided under this heading is in addition to any other transfer authority provided by law.
[Top]
Amounts Available for Obligation
| Source of Funding | FY 2019 Final |
FY 2020 Enacted |
FY 2021 President's Budget* |
| Appropriation2 | $1,870,296 | $2,038,374 | $1,844,865 |
| Mandatory Appropriation (non-add) | |||
| Type 1 Diabetes | (0) | (0) | (0) |
| Other Mandatory financing | (0) | (0) | (0) |
| Rescission | 0 | 0 | 0 |
| Sequestration | 0 | 0 | 0 |
| Secretary's Transfer | -5,001 | 0 | 0 |
| Subtotal, adjusted appropriation | $1,865,295 | $2,038,374 | $1,844,865 |
| OAR HIV/AIDS Transfers | 6,390 | 4,592 | 0 |
| HEAL Transfer from NINDS | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | $1,871,685 | $2,042,966 | $1,844,865 |
| Unobligated balance, start of year3 | 0 | 2,022 | 0 |
| Unobligated balance, end of year3 | -2,022 | 0 | 0 |
| Subtotal, adjusted budget authority | $1,869,663 | $2,044,988 | $1,844,865 |
| Unobligated balance lapsing | -10 | 0 | 0 |
| Total obligations | $1,869,653 | $2,044,988 | $1,844,865 |
1 Excludes the following amounts for reimbursable activities carried out by this account: FY 2019 - $5,439 FY 2020 - $10,050 FY 2021 - $10,050
2 Of which $57.5 million in FY 2019, $70.0 million in FY 2020, and $50.0 million in FY 2021 is derived by transfer from the NIH Innovation Account under the 21st Century Cures Act.
3 Reflects 21st Century Cures Act funding not obliged in FY2019, and carried over into FY 2020
[Top]
Budget Mechanism - Total
| Mechanism | FY 2019 Final | FY 2020 Enacted | FY 2021 Presidents Budget | FY 2021 +/- FY 2020 Enacted | ||||
| No. | Amount | No. | Amount | No. | Amount | No. | Amount | |
| Research Projects | ||||||||
| Noncompeting | 1,504 | $815,909 | 1,643 | $904,108 | 1,683 | $921,029 | 40 | $16,921 |
| Administrative Supplements | (127) | 17,686 | (118) | 16,389 | (107) | 14,889 | (-11) | -1,500 |
| Competing | ||||||||
| Renewal | 49 | 29,371 | 54 | 32,177 | 34 | 20,078 | -20 | -12,100 |
| New | 603 | 377,304 | 666 | 416,042 | 449 | 262,227 | -217 | -153,814 |
| Supplements | 1 | 213 | 1 | 233 | 1 | 146 | 0 | -88 |
| Subtotal Competing | 653 | $406,888 | 721 | $448,453 | 484 | $282,451 | -237 | -$166,002 |
| Subtotal RPGs | 2,157 | $1,240,483 | 2,364 | $1,368,950 | 2,167 | $1,218,368 | -197 | -$150,581 |
| SBIR/STTR | 96 | 57,338 | 109 | 64,358 | 95 | 56,288 | -14 | -8,070 |
| Research Project Grants | 2,253 | $1,297,821 | 2,473 | $1,433,308 | 2,262 | $1,274,656 | -211 | -$158,652 |
| Research Centers | ||||||||
| Specialized/Comprehensive | 27 | $67,412 | 38 | $69,659 | 35 | $63,385 | -3 | -$6,274 |
| Clinical Research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biotechnology | 0 | 50 | 0 | 50 | 0 | 50 | 0 | 0 |
| Comparative Medicine | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Research Centers in Minority Institutions | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Research Centers | 27 | $67,462 | 38 | $69,709 | 35 | $63,435 | -3 | -$6,274 |
| Other Research | ||||||||
| Research Careers | 339 | $56,551 | 357 | $58,523 | 355 | $58,230 | -2 | -$293 |
| Cancer Education | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cooperative Clinical research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biomedical Research Support | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Minority Biomedical Research Support | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other | 67 | 43,367 | 89 | 53,647 | 76 | 45,885 | -13 | -7,762 |
| Other Research | 406 | $99,918 | 446 | $112,170 | 431 | $104,115 | -15 | -$8,055 |
| Total Research Grants | 2,686 | $1,465,201 | 2,957 | $1,615,817 | 2,728 | $1,442,207 | -229 | -$172,980 |
| Ruth L. Kirschstein Training Awards | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 218 | $10,234 | 225 | $10,657 | 224 | $10,604 | -1 | -$53 |
| Institutional Awards | 287 | 28,052 | 490 | 29,004 | 488 | 28,859 | -2 | -145 |
| Total Research Training | 505 | $38,286 | 715 | $39,661 | 712 | $39,463 | -3 | $198 |
| Research and Develop Contracts | 0 | $85,112 | 133 | $82,550 | 132 | $81,724 | -1 | -$825 |
| (SBIR/STTR)(non-add) | (0) | (643) | (0) | (643) | (0) | (643) | (0) | (0) |
| Intramural Research | 278 | 194,848 | 296 | 210,745 | 296 | 191,389 | 0 | -19,356 |
| Res. Management and Support | 259 | 88,239 | 267 | 94,823 | 267 | 90,081 | 0 | -4,741 |
| Res. Management and Support (SBIR Admin) (non-add) | (0) | (216) | (0) | (216) | (0) | (216) | (0) | (0) |
| Construction | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Buildings and Facilities | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total NIMH | 537 | $1,871,685 | 563 | $2,042,966 | 563 | $1,844,865 | 0 | -$198,101 |
1 All items in italics and brackets are non-add entries
2 Of which $57.5 million in FY 2019, $70.0 million in FY 2020, and $50.0 million in FY 2021 is derived by transfer from the NIH Innovation Account under the 21st Century Cures Act
3 Reflects 21st Century Cures Act funding not obliged in FY2019, and carried over into FY 2020
[Top]
Major Changes in the Fiscal Year 2021 President’s Budget Request
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanism and activity details and these highlights will not sum to the total change for FY 2021 President’s Budget request for NIMH. The FY 2021 President’s Budget request is $1,844.9 million, a decrease of $198.1 million compared to the FY 2020 Enacted Level.
Research Project Grants (-$158.7 million; total $1,274.7 million)
Non-competing Research Project Grants funding has increased by $16.9 million. Competing Research Project Grants has decreased by 237 grants or $166.0 million. This reduction is distributed across all programmatic areas and basic, translational or clinical research.
Research Centers (-$6.3 million; total $63.4 million)
This budget activity has decreased by $6.3 million and will continue to fund research studies conducted by extramural universities and institutions.
Intramural Research Programs (-$19.4 million; total $191.4 million)
This budget activity has decreased by $19.4 million and will continue to fund innovative research studies conducted by the Institute’s intramural scientists.
Research Management and Support (-$4.7 million; total $90.1 million)
This budget activity has decreased by $4.7 million and will continue to support the oversight and management of scientific programs critical to fulfilling the Institute’s mission.
[Top]
Summary of Changes
| FY 2020 Enacted | $2,042,966 | |||
| FY 2021 President's Budget | $1,844,865 | |||
| Net change | -$198,101 | |||
| CHANGES | FY 2021 President's Budget | Change from FY2020 Enacted | ||
| FTEs | Budget Authority | FTEs | Budget Authority | |
| A. Built-in | ||||
| 1. Intramural Research: | ||||
| a. Annualization of January 2020 pay increase & benefits | $75,463 | $485 | ||
| b. January FY 2021 pay increase & benefits | 75,463 | 1,118 | ||
| c. Paid days adjustment | 75,463 | -281 | ||
| d. Differences attributable to change in FTE | 75,463 | 0 | ||
| e. Payment for centrally furnished services | 9,760 | -1,755 | ||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | 106,167 | 1,144 | ||
| Subtotal | $711 | |||
| 2. Research Management and Support: | ||||
| a. Annualization of January 2020 pay increase & benefits | $46,051 | $295 | ||
| b. January FY 2021 pay increase & benefits | 46,051 | 700 | ||
| c. Paid days adjustment | 46,051 | -172 | ||
| d. Differences attributable to change in FTE. | 46,051 | 0 | ||
| e. Payment for centrally furnished services | 4,787 | -604 | ||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | 39,244 | 411 | ||
| Subtotal | $629 | |||
| Subtotal, Built-in | $1,340 | |||
[Top]
| CHANGES | FY 2021 President's Budget | Change from FY 2020 Enacted | ||
| No. | Amount | No. | Amount | |
| B. Program: | ||||
| 1. Research Project Grants: | ||||
| a. Noncompeting | 1,683 | $935,918 | 40 | $15,421 |
| b. Competing | 484 | 282,451 | -237 | -166,002 |
| c. SBIR/STTR | 95 | 56,288 | -14 | -8,070 |
| Subtotal, RPGs | 2,262 | $1,274,656 | -211 | -$158,652 |
| 2. Research Centers | 35 | $63,435 | -3 | -$6,274 |
| 3. Other Research | 431 | 104,115 | -15 | -8,055 |
| 4. Research Training | 712 | 39,463 | -3 | -198 |
| 5. Research and development contracts | 132 | 81,724 | -1 | -825 |
| Subtotal, Extramural | $1,563,394 | -$174,004 | ||
| FTEs | FTEs | |||
| 6. Intramural Research | 296 | $191,389 | 0 | -$20,067 |
| 7. Research Management and Support | 267 | 90,081 | 0 | -5,370 |
| 8. Construction | 0 | 0 | ||
| 9. Buildings and Facilities | 0 | 0 | ||
| Subtotal, Program | 563 | $1,844,865 | 0 | -$199,941 |
| Total Changes | -$198,101 | |||
[Top]
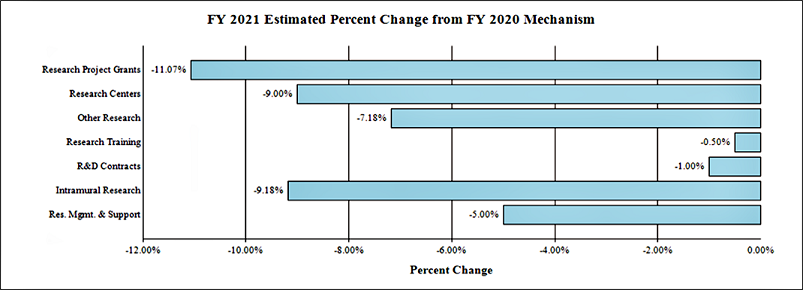
Fiscal Year 2021 Budget Graphs
History of Budget Authority and FTEs:
Distribution by Mechanism:
Change by Selected Mechanism:
[Top]
Budget Authority by Activity
| FY 2019 Final | FY 2020 Enacted | FY 2021 President’s Budget | FY 2021 +/- FY2020 | |||||
| Extramural Research | FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount |
| Detail | ||||||||
| Neuroscience & Basic Behavioral Science | $763,649 | $840,018 | $756,314 | -$83,705 | ||||
| Services & Intervention Research | 142,982 | 157,660 | 141,609 | -16,051 | ||||
| Translational Research | 456,566 | 503,434 | 452,810 | -51,254 | ||||
| AIDS Research | 168,549 | 173,598 | 156,986 | -16,612 | ||||
| Office of the Director | 56,852 | 62,688 | 56,306 | -6,382 | ||||
| Subtotal, Extramural | $1,588,598 | $1,737,398 | $1,563,394 | -$174,004 | ||||
| Intramural Research | 278 | $194,848 | 296 | $210,745 | 296 | $191,389 | 0 | -$19,356 |
| Research Management & Support | 259 | $88,239 | 267 | $94,823 | 267 | $90,081 | 0 | -$4,741 |
| TOTAL | 537 | $1,871,685 | 563 | $2,042,966 | 563 | $1,844,865 | 0 | -$198,101 |
1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
[Top]
Authorizing Legislation
| PHS Act/ Other Citation | U.S. Code Citation | 2019 Amount Authorized | FY 2019 Enacted | 2020 Amount Authorized | FY 2020 President’s Budget | |||
| Research and Investigation | Section 301 | 42§241 | Indefinite | $2,042,966,000 | Indefinite | $1,844,865,000 | ||
| National Institute of Mental Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||||
| Total Budget Authority | $2,042,966,000 | $1,844,865,000 | ||||||
[Top]
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation |
|---|---|---|---|---|
| 2012 | $1,517,006,000 | $1,517,006,000 | $1,460,671,000 | $1,483,068,000 |
| Rescission | $2,802,999 | |||
| 2013 | $1,479,204,000 | $1,483,687,000 | $1,480,265,001 | |
| Rescission | $2,960,530 | |||
| Sequestration | ($74,299,124) | |||
| 2014 | $1,465,782,000 | $1,456,041,000 | $1,446,172,000 | |
| Rescission | $0 | |||
| 2015 | $1,440,076,000 | 1,463,036,000 | ||
| Rescission | $0 | |||
| 2016 | $1,489,417,000 | $1,512,401,000 | $1,520,260,000 | $1,548,390,000 |
| Rescission | $0 | |||
| 2017[1] | $1,518,673,000 | $1,599,747,000 | $1,619,537,000 | $1,601,931,000 |
| Rescission | $0 | |||
| 2018[2] | $1,244,901,000 | $1,668,461,000 | $1,724,568,000 | $1,754,775,000 |
| Rescission | $0 | |||
| 2019[2] | $1,612,192,000 | $1,790,231,000 | $1,871,250,000 | $1,870,296,000 |
| Rescission | $0 | |||
| 2020[2] | $1,630,422,000 | $1,961,704,000 | $2,076,244,000 | $2,038,374,000 |
| Rescission | $0 | |||
| 2021[2] | $1,844,865,000 |
1 Budget Estimate to Congress includes mandatory financing.
2 Includes funds derived by transfer from the NIH Innovation Account under the 21st Century Cures Act
[Top]
Justification of Budget Request
National Institute of Mental Health
Authorizing Legislation:
Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2019 Actual | FY 2020 Enacted | FY 2021 President’s Budget | FY 2021 +/- FY 2020 | |
| BA | $1,871,684,999 | $2,042,966,000 | $1,844,865,000 | -$198,101,000 |
| FTE | 537 | 563 | 563 | 0 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
[Top]
Director’s Overview
The National Institute of Mental Health (NIMH) is the lead federal agency for research on mental illnesses, with a mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure.
In the United States, an estimated 47.6 million adults suffer from a mental illness, which may be significantly impairing and life-threatening.1 Mental disorders are the fourth leading cause of disability in the United States, accounting for 7.1 percent of all disability-adjusted life years.2 One of the most tragic outcomes of untreated mental illness is suicide. Suicide accounts for the loss of over 47,000 American lives each year; it is the second leading cause of death in youth and young adults aged 10-34, and the tenth leading cause of death overall.3
NIMH supports a diverse portfolio of basic, translational, and clinical research, with the potential to improve clinical care over the short, medium, and long-term. To optimize its scientific investments across the long arc of mental health research, NIMH is guided by its Strategic Plan for Research. NIMH is currently revising this Plan to build on the successes of previous plans, provide a framework for research to leverage new opportunities for scientific exploration, and address new challenges in mental health. The new NIMH Strategic Plan for Research, which will be released in 2020, will provide a broad roadmap for the Institute’s research priorities over the next five years.
Where Were We 20 Years Ago?
NIMH helped usher in the 1990s “Decade of the Brain,” laying the initial groundwork for NIMH-supported biological and genetic research on mental illnesses.4 By 2000, neuroscience research had yielded significant advances in developmental neurobiology; molecular genetics; and in understanding the neurotransmitters, receptors, and cytokines in brain disorders.5 The remarkable strides made during this era provided the foundation for the accelerated discovery in neuroscience seen today via novel programs such as the NIH Brain Research through Innovative Neurotechnologies® (BRAIN) Initiative.
Twenty years ago, NIMH supported the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Study, a nationwide public health-focused clinical trial that compared the effectiveness of older (available since the 1950s) ‘typical’ and newer (available since 1990) ‘atypical’ antipsychotic medications used to treat schizophrenia.6 CATIE was the largest, longest, and most comprehensive independent trial ever to examine existing therapies for schizophrenia. The aim of the CATIE study was to determine which medications provide the best treatment for schizophrenia. Clozapine, an atypical antipsychotic drug, was confirmed as the most effective drug for individuals with a poor symptom response to other antipsychotic medications, although clozapine was also associated with adverse side effects. To this day, clozapine remains the only antipsychotic that is indicated for treatment-resistant schizophrenia.
In the early 2000s, NIMH also supported the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) Study to examine the effectiveness of different treatments for people with major depression who had not responded to initial treatment with an antidepressant.7 This was the largest and longest study ever conducted to evaluate depression treatment. STAR*D provided up to four treatment steps per patient and was designed to give guidance in selecting the best next-step treatment for the many patients who fail to get sufficient relief from their initial antidepressant. STAR*D investigators found no significant group differences between any of 11 drug combination treatments. An overall analysis of the STAR*D results indicates that patients with difficult-to-treat depression can get well after trying several treatment strategies, but the odds of beating the depression diminish with every additional treatment strategy needed.8,9 The results of STAR*D also underscored the need for more effective treatment strategies and more patient-tailored interventions for the treatment of major depression.
Based in part on decades of NIMH-supported research, strong evidence has amassed for psychotherapies, such as cognitive behavioral therapy (CBT) and applied behavioral analysis (ABA). As an example, CBT was designed for depression and anxiety as a short-term therapy that focuses on changing thought processes that produce negative feelings. Cognitive therapy has proven as effective as medication in alleviating depression and even more effective in reducing relapse and recurrence.10 In fact, NIMH-funded research not only demonstrated the
effectiveness of CBT but established a new standard for the field of psychotherapy. As another example, ABA is an intervention for autism based on behaviorist theory that desired behaviors can be taught through a system of rewards and consequences. Research in the 1990s demonstrated the efficacy of ABA, and this intervention is now a mandated service covered in most states.11,12
Where Are We Today?
Advances in neuroscience over the past decade, in part through the NIH BRAIN Initiative, have provided tools to look deeply into the function of neural circuits, and directly test hypotheses about brain-behavior relationships using noninvasive brain stimulation technologies. Researchers have also developed incredible technologies to measure and modulate the activity of specific circuits, such as optogenetics, chemogenetics, viral tracing, and high-resolution optical imaging. Today, noninvasive neuromodulation devices allow scientists to change function within circuits for therapeutic benefit. For example, this approach led to the Food and Drug Administration (FDA) approval of transcranial magnetic stimulation (TMS) for the treatment of depression and obsessive-compulsive disorder.13 TMS, which was originally a tool to study brain function, was first tested as a therapeutic intervention in the NIMH intramural research program.14
In FY 2019, the FDA approved two treatments that were based on research conducted by NIMH researchers. The first technology derived from the NIMH’s intramural research patent portfolio to receive FDA approval was esketamine nasal spray medication for treatment-resistant depression.15 While typical antidepressants may take weeks to work, ketamine dramatically reduces depressive symptoms within hours.16 The FDA approved brexanolone intravenous infusion, the first-ever drug specifically designed to treat postpartum depression,17which impacts 1 in 9 women in the United States.18 Research conducted in the 1980s in the NIMH’s intramural research program contributed to the formulation of this new therapy.19
Given the troubling rise in the national suicide rate in the past decades, suicide prevention research is an urgent priority for NIMH. As such, NIMH is supporting suicide prevention efforts in healthcare settings. Nearly half of individuals who die by suicide had some type of medical visit in the 30 days prior to death, and around 80 percent did so in the year before death.20,21 NIMH research has identified a growing number of evidence-based suicide prevention tools that can be implemented in the healthcare system. NIMH-funded research shows that screening all patients doubles the number of people that can be identified as needing help for suicide risk.22 NIMH is also supporting studies testing the best ways to deliver evidence-based interventions, such as Safety Planning, in various settings and populations.23 Safety Planning is an approach that reduces access to lethal means, identifies coping strategies to decrease risk of suicidal behavior, and lists people and resources that could help in crisis. NIMH-funded researchers have shown that this combination of screening, brief intervention, and follow-up contact reduced suicide attempts in the next year by about 30 percent.24 To build on these findings, NIMH continues to support research aimed at identifying who is most at risk for suicide, understanding the causes of suicide risk, developing interventions, and testing the effectiveness of suicide prevention services in real-world settings.
Since NIMH launched the Recovery After an Initial Schizophrenia Episode (RAISE) project over a decade ago, researchers have made tremendous progress on early intervention services for people in the United States experiencing first episode psychosis, with an emphasis on coordinated specialty care (CSC).25 The RAISE project demonstrated that early intervention improves clinical outcomes among youth with first episode psychosis, including members of racial and ethnic minority groups, and that CSC is a feasible and cost-effective approach to early intervention for these individuals.26,27,28,29 Through collaborations with other federal agencies, NIMH has transformed these findings into real-world change. CSC is now the standard of care for early psychosis, with over 280 CSC programs across the country. RAISE has helped approximately 17,000 young people confronting the tremendous challenge of a first episode of psychosis by ensuring they have access to the best possible evidence-based care.
What Are We Investing in for the Future?
Building on the findings of RAISE and in support of expanding CSC programs across the United States, NIMH established the Early Psychosis Intervention Network (EPINET).30 EPINET aims to create an early psychosis “learning healthcare system,” in which data that are routinely collected in CSC programs as part of clinical practice drive continuous improvement in patient care and scientific discovery. NIMH recently funded five regional scientific hubs and one national data coordinating center that will standardize, collect, and aggregate data across community clinics and use computational methods to study CSC fidelity, quality, and treatment effectiveness.31 By studying large, nationally representative data sets, EPINET may provide crucial insights into how best to tailor early psychosis care for individuals and provide information to guide improvements in diagnosis and intervention.
Circuit neuroscience holds great promise for impact on mental health in the future. As noted above, neuroscience has undergone a revolution over the past decade with the advent of myriad technologies aimed at measuring and modulating the activity of specific circuits. Circuit neuroscience may enable diagnostic and treatment strategies that normalize the circuit dysfunctions that underlie psychiatric disorders. To drive progress in circuit neuroscience, NIMH supports cutting-edge research that seeks to reveal how brain cells and complex neural circuits dynamically interact to influence mental functions.
Even though autism spectrum disorder (ASD) can be diagnosed as early as two years of age, most children are not diagnosed until after their fourth birthday.32 Screening children in primary care settings could help identify those at high risk for ASD, enabling early intervention and better long-term outcomes. As such, NIMH is supporting efforts to identify ASD at the earliest age possible. For example, NIMH funds the ASD Prevention, Early Detection, Engagement, and Services Research (ASD PEDS) Network, which comprises five separate but coordinated studies to test strategies for universal screening and early treatment.33 NIMH-funded research has identified risk markers within the first 12 months of age.34 Yet, a critical gap exists in translating these methods into practical, efficient, and inexpensive screening tools that could be implemented in the general population and within pediatric primary care settings. NIMH is encouraging research to develop and validate new screening methods for ASD that can be used in infancy.35
The healthcare landscape in the United States is constantly changing. To keep pace with these changes and address gaps between research and practice, NIMH published a funding opportunity announcement, A Practice-Based Research Network to Transform Mental Health Care: Science, Service Delivery and Sustainability.36 The initiative aims to transform the development, delivery, and sustainability of evidenced-based mental health practices and services in the United States. Specifically, this innovative approach provides the infrastructure that can be leveraged to support comparative effectiveness trials; harmonize electronic health record data across multiple integrated systems for common analyses; enable scientists to study rare events (e.g., suicide, ASD, first episode psychosis) by using and advancing innovative methodologies (e.g., predictive analytics); and, develop, test, and deploy large-scale mental health information technology interventions, generating data that will fuel the transformation of mental health care.
Overall Budget Policy: The FY 2021 President’s Budget request is $1,844.9 million, a decrease of $198.1 million or 9.7 percent compared to the FY 2020 Enacted level.
Program Descriptions
Office of the Director
The NIMH Office of the Director (OD) leads the Institute in implementing the NIMH mission to transform the understanding and treatment of mental illnesses. The OD provides scientific leadership, sets programmatic priorities, coordinates cross-cutting programs, determines Institute policy, and provides overall administrative and operational coordination for the Institute. The OD houses nine offices: Office on AIDS; Office of Autism Research Coordination; Office of Clinical Research; Office of Genomics Research Coordination; Office for Disparities Research and Workforce Diversity; Office of Management; Office of Rural Mental Health Research; Office of Science Policy, Planning, and Communications; and, Office of Technology Development and Coordination. Each of the offices within the OD play an important role in supporting the Institute.
As an example of research funded by OD, NIMH is planning to launch an initiative supporting projects aimed at implementing and sustaining evidence-based mental health practices in low-resource settings to achieve equity in outcomes.37 Limited capital and human resources can create barriers to care delivery. The initiative would encourage innovative approaches to remediate barriers to provision, receipt, and/or benefit from evidence-based practices. Studies may also generate new information about factors integral to achieving equity in mental health outcomes, with due consideration for the needs of individuals across the life span. The ultimate goal of the initiative is to improve mental health outcomes for underserved populations and reduce or eliminate health disparities.
Budget Policy: The FY 2021 President’s Budget request is $56.3 million, a decrease of $6.4 million or 10.2 percent compared to the FY 2020 Enacted level.
Neuroscience and Basic Behavioral Science
The Division of Neuroscience and Basic Behavioral Science (DNBBS) provides support for research in the areas of basic neuroscience, genetics, integrative neuroscience, research training, resource development, and drug discovery. In cooperation with other NIMH programs and the wider research community, this program ensures that relevant basic scientific knowledge is generated and used in pursuit of improved methods that, in the long term, could be used to diagnose, treat, and prevent mental illnesses.
DNBBS funds grants across a range of research topics to enhance understanding of the basic neurobiology underlying mental illnesses. In FY 2021, DNBBS plans to support research to develop and validate behavioral measures in humans that can provide a readout of the brain subsystems relevant to anhedonia, a key symptom of major depression as well as other mental illnesses. In addition, DNBBS will support tool-development projects to further elucidate signals from the human genome that point to susceptibility to mental illnesses.
Program Portrait: Using Genetic Fine Mapping to Identify Causal Genetic Contributors to Mental Illnesses
Tremendous progress has been made in understanding the role of genetics in the development of mental illnesses. Genome-wide association studies (GWAS) have uncovered links between certain variations in the genetic code and features of psychiatric disorders, including schizophrenia, autism, and depression. These links are mostly statistical relationships between common variations in the building blocks of DNA (called nucleotides) and a trait of interest. An immediate barrier to translating genetic associations into causal disease mechanisms is the uncertain relationship between these statistically identified genetic variations and the molecular changes that can result from them. Fine-mapping procedures aim to overcome this barrier by leveraging information about gene expression patterns and their functional impacts to determine which genetic variations in a genomic region of interest are most likely to be causally related to a trait.
NIMH encourages research to develop and apply resources and tools for the large-scale and systematic genetic fine-mapping of serious mental illnesses and related traits.38 Such traits include disease status, as well as molecular features in neural tissues and cell types. Proposed studies may generate new data or use existing population-scale human data from groups with diverse ancestries. The ultimate goal is to provide the research community with high-confidence information on causal genetic contributors to allow for deeper insights into disease mechanisms.
Budget Policy: The FY 2021 President’s Budget request is $756.3 million, a decrease of $83.7 million or 10.0 percent compared to the FY 2020 Enacted level.
Translational Research
The Division of Translational Research (DTR) supports integrative, multidisciplinary research and training programs that translate findings from basic science to discover the causes, mechanisms, and trajectories of mental illnesses, and develop effective interventions for individuals across the lifespan. DTR supports research using various forms of scientific analysis, including computational psychiatry and machine learning to elucidate the characteristics of, and risk factors for, mental illnesses; the neurobehavioral mechanisms of psychopathology; the trajectories of risk and resilience based on the interactive influences of genetics, brain development, environment, and experience; and, the design and testing of innovative treatments and interventions. As such, DTR-supported research efforts may have intermediate-term impact and pave the way towards effective treatment and prevention for mental illnesses.
One area of high priority for DTR is to improve outcomes for individuals exposed to trauma. Such outcomes may include post-traumatic stress disorder (PTSD), depression, insomnia, pain, substance use disorders, and suicide. A major gap in knowledge has been the lack of means to predict who will experience adverse outcomes from trauma before these outcomes occur, which would enable effective prevention strategies. To address this gap, NIMH, the Department of Defense, private foundations, and industry are funding the Aurora study to support the development of effective treatments and preventions that could improve understanding of trauma outcome predictors.39 This landmark study with 5,000 participants across the United States will inform the development of predictive and diagnostic biomarkers that are needed to treat and prevent adverse outcomes in civilian and military veterans. In addition, DTR is supporting research using advanced digital techniques, including natural language processing, machine learning, and predictive coding, that aim to predict mental health outcomes, such as risk for suicide.40,41 DTR also supports work harnessing the latest advances in artificial intelligence to advance mechanistic understanding of how circuits in the brain shape behavior.42
Program Portrait: Using Opportunities for Invasive Neural Recording and Brain Stimulation in Humans to Advance Our Understanding of the Neural Circuitry of Mental Illnesses
Invasive neural recordings can be used to explore the neural circuitry underlying complex moods, emotions, and behaviors with high spatial and temporal precision. Additionally, stimulation of the brain using implanted electrodes allows researchers to directly test hypotheses to better understand the structure and dynamics of neural networks. Together, invasive neural recordings and brain stimulation provide opportunities for researchers to understand which neural circuits are involved in complex behaviors in humans, and how to alter dysfunctional circuits into functional states, informing both invasive and non-invasive brain stimulation therapies of the future.
NIMH is encouraging researchers to use invasive neural recording and brain stimulation opportunities in humans to study the neural circuity underlying mental illnesses.43 These opportunities arise during the normal treatment course of a variety of clinical conditions, such as when patients undergo deep brain stimulation surgery for Parkinson’s disease, when patients are monitored for epilepsy using electrocorticography, or when patients receive chronic brain implants for non-mental health and mental health-related conditions. Many people receiving these procedures may also have mental health diagnoses. Researchers must also consider patient privacy and ethical considerations, in maximizing benefit while minimizing risk to patients. Careful study of fluctuating mood patterns in patients with and without a mental illness can provide unique insights into the neural circuits that drive human behavior.
Budget Policy: The FY 2021 President’s Budget request is $452.2 million, a decrease of $51.3 million or 10.2 percent compared to the FY 2020 Enacted level.
Services and Intervention Research
The Division of Services and Intervention Research (DSIR) supports research that evaluates the effectiveness of psychosocial, pharmacological, somatic, rehabilitative, and combined interventions to prevent or treat mental illnesses. DSIR refines and evaluates treatment and preventive interventions for children, adolescents, and adults, focusing on acute and long-term symptom reduction, remission, and improved community functioning. DSIR also supports mental health services research, including interventions to improve the quality and outcomes of care; organization- and system-level interventions to enhance service delivery; and, strategies for widespread dissemination and implementation of evidence-based treatments into routine care settings. DSIR funds studies that are designed to have near-term impact, targeted at improving care for patients currently suffering from mental illnesses.
DSIR initiatives encourage practice-based research with near-term potential for improving intervention effectiveness and service delivery, as illustrated by the ALACRITY Research Center program (Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness).44,45 These centers incorporate a variety of transdisciplinary collaborations and prioritize a deployment-focused approach to yield interventions and service strategies that are relevant and can be rapidly integrated into practice. Many of the centers capitalize digital health platforms and data science methods to learn about mental illness onset and progression in clinical populations, improve diagnosis, and deliver targeted interventions via smart communication technologies. The centers also account for the perspectives of a variety of stakeholders, including patients, families, providers, and more. The currently funded ALACRITY Centers span a variety of key populations and practice settings; cover a range of science, spanning intervention refinement and optimization through implementation and services research; and, incorporate a variety of transdisciplinary collaborations.
Program Portrait: Telehealth to Optimize Mental Health Care for Emergency Department Patients at Risk for Suicide
Emergency departments (EDs) are critical settings for suicide preventive efforts. In the United States, there are nearly half a million visits to EDs for self-harm, and many more visits that involve suicide ideation.46 Research finds that existing ED providers identify only half of all patients at risk for suicide, many of whom could benefit from evidence-based care practices.47 These care practices include: universal risk detection efforts that can double the number of individuals identified to be in need of suicide prevention treatment;2,48 brief interventions such as the Safety Planning Intervention; and, follow-up telephone contacts that have resulted in fewer repeat suicide attempts (30 to 50 percent reduction).49,50
There is a shortage of ED-based mental health providers. Some EDs have begun to address this shortage by using telehealth to bring more mental health specialists into these health care settings, but questions remain regarding how telehealth services for suicide prevention care affect ED workflows. In particular, it is not known how telehealth is currently used to address suicide risk among ED patients; and, most importantly, it is not known whether telehealth-provided ED suicide prevention services are related to patients’ immediate, as well as longer-term, suicide morbidity and mortality outcomes. NIMH is encouraging research to identify feasible approaches to telehealth-supplied suicide prevention practices. Of particular interest is whether this approach improves patients’ outcomes related to suicide (including intentional and non-intentional injuries and mortality) and increases their use of health care services.51
Budget Policy: The FY 2021 President’s Budget request is $141.6 million, a decrease of $16.1 million or 10.2 percent compared to the FY 2020 Enacted level.
AIDS Research
The Division of AIDS Research (DAR) supports research and research training that addresses the priority areas outlined in the NIH HIV/AIDS Research Priorities and Guidelines for Determining AIDS Funding.52 DAR-supported research includes behavioral and social science studies aimed at reducing HIV/AIDS incidence through the development, testing, and implementation of new and improved prevention strategies, improving health outcomes of those living with HIV through improved linkage to care, and adherence to effective treatments. DAR also supports research to understand, prevent, and treat the neurological dysfunction associated with HIV infection. DAR is participating in cure research by supporting studies to eradicate or silence the HIV virus from biological reservoirs in the central nervous system (CNS), where the virus may evade detection and treatment. HIV latency in the CNS is critically important to consider in studies of eradication and reactivation. Many drugs designed to eradicate the virus are unable to penetrate the CNS, because the CNS acts as a protective reservoir for HIV. This work may also inform methods to prevent or treat the neurological comorbidities of HIV, such as cognitive and behavioral impairments, with targeted research to understand HIV-induced neurological pathology, with emphasis on long-term antiretroviral therapy.
DAR research also places special emphasis on World Health Organization-defined key populations, health disparities, and the impact of mental illnesses that may increase the risk for contracting HIV or negatively impact the health outcomes of those living with HIV. Additionally, DAR ensures effective integration of biomedical approaches and multidisciplinary expertise are considered in agency-wide planning efforts, to help achieve an AIDS-free generation.
Budget Policy: The FY 2021 President’s Budget request is $157.0 million, a decrease of $16.6 million or 9.6 percent compared to the FY 2020 Enacted level.
Intramural Research Programs
The Division of Intramural Research Programs (IRP) is the internal research component of NIMH, complementing the Institute’s extramural grant funding program. IRP scientists investigate basic, translational, and clinical aspects of brain function and behavior, conducting state-of-the-art research using unique NIH resources. In addition, the IRP provides an excellent environment for training the next generation of clinical and basic scientists.
IRP researchers are currently investigating innovative behavioral treatments and medications for children with severe mood dysregulation or anxiety and are using computational and multimodal neuroimaging approaches to understand adolescent depression. Recently, intramural researchers used functional magnetic resonance imaging (fMRI) to identify differences in how the brains of irritable youth react to frustration. In another fMRI study, researchers revealed differences in brain activity in children with anhedonia. People who experience anhedonia have lost interest and pleasure in activities they used to enjoy.53 IRP scientists continue to explore novel medications for treatment-resistant depression in adults, including ketamine and other experimental fast-acting antidepressant medications, and are working to understand the neurobiological underpinnings of suicide. NIMH scientists also continue to investigate post-infectious neuroimmune disorders, including Pediatric Acute-onset Neuropsychiatric Syndrome (PANS) and PAN Disorder Associated with Streptococcal infection (PANDAS). These syndromes are characterized by a sudden onset of obsessive-compulsive disorder and/or severe eating restrictions, and associated characteristic cognitive, behavioral or neurological symptoms.54 Recent work in this area includes investigations into treatment options, as well as a nationwide effort to obtain prospective, longitudinal clinical information and samples and genetic material from children with PANS and their families.55
Budget Policy: The FY 2021 President’s Budget request is $191.4 million, a decrease of $19.4 million or 9.2 percent compared to the FY 2020 Enacted level.
Research Management and Support (RMS)
Research Management and Support (RMS) activities provide administrative, budgetary, logistical, and scientific support in the review, award, and monitoring of research and training grants, and research and development contracts. RMS functions include strategic planning, coordination, and evaluation of NIMH programs, regulatory compliance, coordination of global mental health efforts, and liaising with other Federal agencies, Congress, and the public. Through RMS activities, NIMH continues to provide accountability and administrative support for meritorious basic, clinical, and translational research and continues to promote health information dissemination, education, and outreach activities.
Budget Policy: The FY 2021 President’s Budget request is $90.1 million, a decrease of $4.7 million or 5.0 percent compared to the FY 2020 Enacted level.
Budget Authority by Object Class
| FY 2020 Enacted | FY 2021 President's Budget | FY 2021 +/ - FY 2020 | |
| Total compensable workyears: | |||
| Full-time equivalent | 563 | 563 | 0 |
| Full-time equivalent of overtime and holiday hours | 0 | 0 | 0 |
| Average ES salary | $197 | $201 | $4 |
| Average GM/GS grade | 13.0 | 13.0 | 0.0 |
| Average GM/GS salary | $125 | $127 | $2 |
| Average salary, grade established by act of July 1,1944 (42 U.S.C. 207) | $0 | $0 | $0 |
| Average salary of upgraded positions | $140 | $140 | $1 |
| OBJECT CLASSES | FY 2020 Enacted | FY 2021 President's Budget | FY 2021 +/ - FY 2020 |
| Personnel Compensation | |||
| 11.1 Full-Time Permanent | 50,532 | 51,111 | 580 |
| 11.3 Other Than Full-Time Permanent | 26,501 | 26,805 | 304 |
| 11.5 Other Personnel Compensation | 2,544 | 2,574 | 29 |
| 11.7 Military Personnel | 0 | 0 | 0 |
| 11.8 Special Personnel Services Payments | 11,453 | 11,757 | 303 |
| 11.9 Subtotal Personnel Compensation | $91,031 | $92,246 | $1,216 |
| 12.1 Civilian Personnel Benefits | 28,177 | 29,267 | 1090 |
| 12.2 Military Personnel Benefits | 0 | 0 | 0 |
| 13.0 Benefits to Former Personnel | 0 | 0 | 0 |
| Subtotal Pay Costs | $119,208 | $121,513 | $2,305 |
| 21.0 Travel & Transportation of Persons | 3,546 | 3,052 | -494 |
| 22.0 Transportation of Things | 109 | 93 | -16 |
| 23.1 Rental Payments to GSA | 0 | 0 | 0 |
| 23.2 Rental Payments to Others | 0 | 0 | 0 |
| 23.3 Communications, Utilities & Misc. Charges | 1,028 | 885 | -143 |
| 24.0 Printing & Reproduction | 16 | 13 | -2 |
| 25.1 Consulting Services | 2,581 | 2,255 | -326 |
| 25.2 Other Services | 35,406 | 30,378 | -5,028 |
| 25.3 Purchase of goods and services from government accounts | 176,418 | 161,816 | -14,602 |
| 25.4 Operation & Maintenance of Facilities | 1,611 | 1,368 | -243 |
| 25.5 R&D Contracts | 20,501 | 16,982 | -3,519 |
| 25.6 Medical Care | 80 | 68 | -12 |
| 25.7 Operation & Maintenance of Equipment | 12,723 | 12,116 | -607 |
| 25.8 Subsistence & Support of Persons | 18 | 16 | -3 |
| 25.0 Subtotal Other Contractual Services | $249,339 | $225,000 | -$24,339 |
| 26.0 Supplies & Materials | 6,950 | 5,894 | -1,056 |
| 31.0 Equipment | 7,921 | 6,743 | -1,178 |
| 32.0 Land and Structures | 0 | 0 | 0 |
| 33.0 Investments & Loans | 0 | 0 | 0 |
| 41.0 Grants, Subsidies and Contributions | 1,654,849 | 1,481,670 | -173,179 |
| 42.0 Insurance Claims and Indemnities | 0 | 0 | 0 |
| 43.0 Interest & Dividends | 1 | 1 | 0 |
| 44.0 Refunds | 0 | 0 | 0 |
| Subtotal Non-Pay Costs | $1,923,758 | $1,723,352 | -$200,406 |
| Total Budget Authority by Object Class | $2,042,966 | $1,844,865 | -$198,101 |
1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
[Top]
Salaries and Expenses
(Dollars in Thousands)
| OBJECT CLASSES | FY 2020 Enacted | FY 2021 President's Budget | FY 2021 +/ - FY 2020 |
| Personnel Compensation | |||
| Full-Time Permanent (11.1) | $50,532 | $51,111 | $580 |
| Other Than Full-Time Permanent (11.3) | 26,501 | 26,805 | 304 |
| Other Personnel Compensation (11.5) | 2,544 | 2,574 | 29 |
| Military Personnel (11.7) | 0 | 0 | 0 |
| Special Personnel Services Payments (11.8) | 11,453 | 11,757 | 303 |
| Subtotal Personnel Compensation (11.9) | $91,301 | $92,246 | $1,216 |
| Civilian Personnel Benefits (12.1) | $28,177 | $29,267 | $1,090 |
| Military Personnel Benefits (12.2) | 0 | 0 | 0 |
| Benefits to Former Personnel (13.0) | 0 | 0 | 0 |
| Subtotal Pay Costs | 119,208 | 121,513 | $2,305 |
| Travel & Transportation of Persons (21.0) | $3,546 | $3,052 | -$494 |
| Transportation of Things (22.0) | 109 | 93 | -16 |
| Rental Payments to Others (23.2) | 0 | 0 | 0 |
| Communications, Utilities & Misc. Charges (23.3) | 1,028 | 885 | -143 |
| Printing & Reproduction (24.0) | 16 | 13 | -2 |
| Other Contractual Services: | |||
| Consultant Services (25.1) | 2,581 | 2,255 | -326 |
| Other Services (25.2) | 35,406 | 30,378 | -5,028 |
| Purchases from government accounts (25.3) | 106,374 | 92,111 | -14,263 |
| Operation & Maintenance of Facilities (25.4) | 1,611 | 1,368 | -243 |
| Operation & Maintenance of Equipment (25.7) | 12,723 | 12,116 | -607 |
| Subsistence & Support of Persons (25.8) | 18 | 16 | -3 |
| Subtotal Other Contractual Services | $158,714 | $138,244 | -$20,469 |
| Supplies & Materials (26.0) | $6,950 | $5,894 | -$1,056 |
| Subtotal Non-Pay Costs | $170,362 | $148,182 | -$22,180 |
| Total Administrative Costs | $289,570 | $269,696 | -$19,874 |
[Top]
Detail of Full-Time Equivalent Employment (FTE)
| Office/Division | FY 2019 Final | FY 2020 Enacted | FY 2021 President's Budget | ||||||
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of AIDS Research | |||||||||
| Direct: | 16 | - | 16 | 16 | - | 16 | 16 | - | 16 |
| Reimbursable: | - | - | - | - | - | - | - | ||
| Total: | 16 | - | 16 | 16 | - | 16 | 16 | - | 16 |
| Division of Extramural Activities | |||||||||
| Direct: | 43 | - | 43 | 43 | - | 43 | 43 | - | 43 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 43 | - | 43 | 43 | - | 43 | 43 | - | 43 |
| Division of Intramural Research Programs | |||||||||
| Direct: | 271 | - | 271 | 289 | - | 289 | 289 | - | 289 |
| Reimbursable: | 7 | - | 7 | 7 | - | 7 | 7 | - | 7 |
| Total: | 278 | - | 278 | 296 | - | 296 | 296 | - | 296 |
| Division of Neuroscience and Basic Behavioral Science | |||||||||
| Direct: | 25 | - | 25 | 25 | - | 25 | 25 | - | 25 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 25 | - | 25 | 25 | - | 25 | 25 | - | 25 |
| Division of Services and Intervention Research | |||||||||
| Direct: | 15 | - | 15 | 15 | - | 15 | 15 | - | 15 |
| Reimbursable: | - | - | - | - | - | - | - | ||
| Total: | 15 | - | 15 | 15 | - | 15 | 15 | - | 15 |
| Division of Translational Research | |||||||||
| Direct: | 27 | - | 27 | 27 | - | 27 | 27 | - | 27 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 27 | - | 27 | 27 | - | 27 | 27 | - | 27 |
| Office of the Director | |||||||||
| Direct: | 127 | - | 127 | 136 | - | 136 | 136 | - | 136 |
| Reimbursable: | 6 | - | 6 | 5 | - | 5 | 5 | - | 5 |
| Total: | 133 | - | 133 | 141 | - | 141 | 141 | - | 141 |
| Total | 537 | - | 537 | 563 | - | 563 | 563 | - | 563 |
| Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
| FTE's supported by funds from Cooperative Research and Development Agreements | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fiscal Year | Average GS Grade |
| 2017 | 12.6 |
| 2018 | 12.7 |
| 2019 | 12.8 |
| 2020 | 13.0 |
| 2021 | 13.0 |
[Top]
Detail of Positions
| Grade | FY 2019 Final |
FY 2020 Enacted |
FY 2021 President's Budget |
|---|---|---|---|
| Total, ES Positions | 1 | 1 | 1 |
| Total, ES Salary | 188,243 | 197,272 | 201,271 |
| GM/GS-15 | 70 | 70 | 70 |
| GM/GS-14 | 77 | 77 | 77 |
| GM/GS-13 | 109 | 135 | 135 |
| GS-12 | 77 | 77 | 77 |
| GS-11 | 33 | 33 | 33 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 13 | 13 | 13 |
| GS-8 | 5 | 5 | 5 |
| GS-7 | 7 | 7 | 7 |
| GS-6 | 0 | 0 | 0 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 1 | 1 | 1 |
| GS-3 | 1 | 1 | 1 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 393 | 419 | 419 |
| Grades established by Act of July 1, 1944 (42 U.S.C. 207): | 0 | 0 | 0 |
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 0 | 0 | 0 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 0 | 0 | 0 |
| Ungraded | 174 | 174 | 174 |
| Total permanent positions | 397 | 397 | 397 |
| Total positions, end of year | 568 | 594 | 594 |
| Total full-time equivalent (FTE) employment, end of year | 537 | 563 | 563 |
| Average ES salary | 188,243 | 197,272 | 201,271 |
| Average GM/GS grade | 12.8 | 13.0 | 13.0 |
| Average GM/GS salary | 119,161 | 125,333 | 127,393 |
| 1Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||
1 Substance Abuse and Mental Health Services Administration. (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19‑5068, NSDUH Series H‑54). Retrieved from https://www.samhsa.gov/data/
2 Institute of Health Metrics and Evaluation. http://ghdx.healthdata.org/gbd-results-tool accessed September 2019. http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2017-permalink/abae84a95a64bd733ce16cdc380e82cd
3 CDC, NCIPC. WISQARS: http://www.cdc.gov/injury/wisqars/index.html accessed September 2019.
4 https://www.loc.gov/loc/brain/
5 https://pdfs.semanticscholar.org/e314/bf4dbd43731b67647c321c053d2735c6ae92.pdf
6 https://www.nimh.nih.gov/funding/clinical-research/practical/catie/index.shtml
7 https://www.nimh.nih.gov/funding/clinical-research/practical/stard/index.shtml
8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4314062/
9 https://ps.psychiatryonline.org/doi/full/10.1176/ps.2009.60.11.1439
10 https://reporter.nih.gov/project-details/9538844
11 https://www.ncbi.nlm.nih.gov/pubmed/8427693
12 https://www.autismspeaks.org/health-insurance-coverage-autism
13 https://www.fda.gov/news-events/press-announcements/fda-permits-marketing-transcranial-magnetic-stimulation-treatment-obsessive-compulsive-disorder
14 https://www.ncbi.nlm.nih.gov/pubmed/8547583
15 https://www.fda.gov/news-events/press-announcements/fda-approves-new-nasal-spray-medication-treatment-resistant-depression-available-only-certified
17 https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-post-partum-depression
18 https://www.cdc.gov/mmwr/volumes/66/wr/mm6606a1.htm?s_cid=mm6606a1_w
20 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4026491/
21 https://www.ncbi.nlm.nih.gov/pubmed/12042175
22 https://www.ncbi.nlm.nih.gov/pubmed/26654691
23 https://www.ncbi.nlm.nih.gov/pubmed/29998307
24 https://www.ncbi.nlm.nih.gov/pubmed/28456130
25 https://www.nimh.nih.gov/health/topics/schizophrenia/raise/index.shtml
26 https://www.ncbi.nlm.nih.gov/pubmed/26481174
27 https://www.ncbi.nlm.nih.gov/pubmed/25772764
28 https://www.ncbi.nlm.nih.gov/pubmed/30152275
29 https://www.ncbi.nlm.nih.gov/pubmed/26834024
30 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-19-150.html
32 https://www.cdc.gov/ncbddd/autism/addm-community-report/documents/addm-community-report-2018-h.pdf
33 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-14-100.html
34 https://www.ncbi.nlm.nih.gov/pubmed/28592562
35 https://grants.nih.gov/grants/guide/rfa-files/rfa-mh-19-120.html
36 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-19-225.html
39 https://reporter.nih.gov/project-details/9756462
40 https://www.ncbi.nlm.nih.gov/pubmed/30389840
41 https://www.ncbi.nlm.nih.gov/pubmed/30710497
42 https://grants.nih.gov/grants/guide/pa-files/PAR-19-344.html
44 https://grants.nih.gov/grants/guide/pa-files/PAR-16-354.html
45 https://grants.nih.gov/grants/guide/pa-files/PAR-18-701.html
46 https://webappa.cdc.gov/sasweb/ncipc/nfirates.html
47 https://www.ncbi.nlm.nih.gov/pubmed/26654691
48 https://www.ncbi.nlm.nih.gov/pubmed/15802695
49 https://www.ncbi.nlm.nih.gov/pubmed/28456130
50 https://www.ncbi.nlm.nih.gov/pubmed/29998307
52 https://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-137.html
54 https://www.nimh.nih.gov/health/publications/pandas/index.shtml
