FY 2019 Budget - Congressional Justification
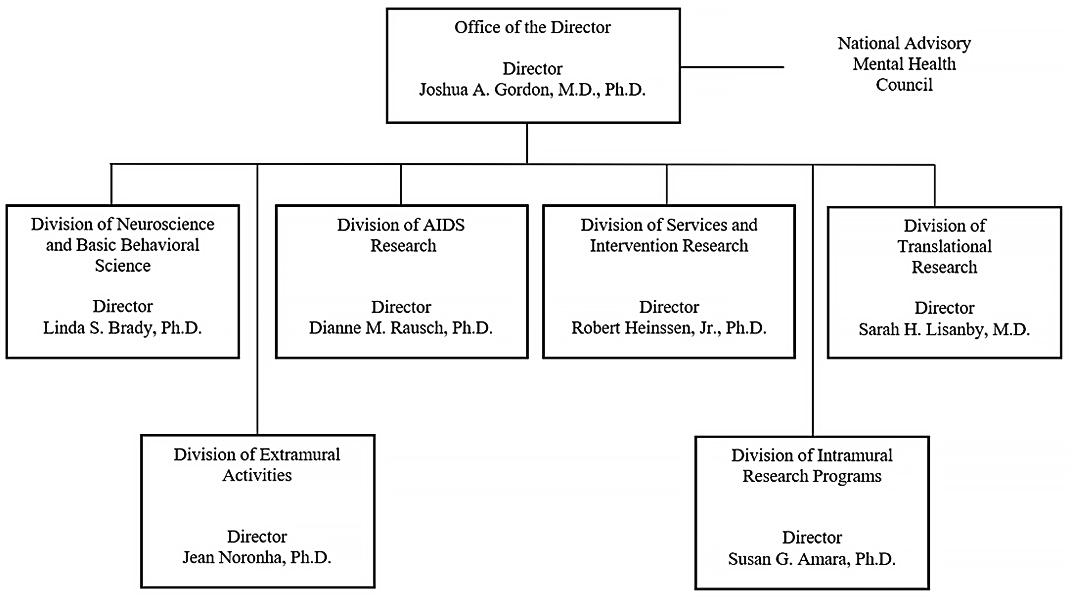
- Organization Chart
- Appropriation Language
- Amounts Available for Obligation
- Budget Graphs
- Authorizing Legislation
- Appropriations History
- Justification of Budget Request
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
Department of Health and Human Services
National Institutes of Health
National Institute of Mental Health
Organization Chart
[Top]
Appropriation Language
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
For carrying out section 301 and title IV of the PHS Act with respect to mental health, $1,554,692,000.
[Top]
Amounts Available for Obligation
| Source of Funding | FY 2017
Final |
FY 2018
Annualized CR |
FY 2019
President's Budget* |
|---|---|---|---|
| Appropriation | $1,601,931 | $1,601,931 | $1,612,192 |
| Mandatory Appropriation (non-add) | |||
| Type 1 Diabetes | (0) | (0) | (0) |
| Other Mandatory financing | (0) | (0) | (0) |
| Rescission | 0 | -10,879 | 0 |
| Sequestration | 0 | 0 | 0 |
| Secretary's Transfer | -3,554 | ||
| Subtotal, adjusted appropriation | $1,598,377 | $1,591,052 | $1,612,192 |
| OAR HIV/AIDS Transfers | 6,281 | 0 | 0 |
| Subtotal, adjusted budget authority | $1,604,658 | $1,591,052 | $1,612,192 |
| Unobligated balance, start of year | 0 | 0 | 0 |
| Unobligated balance, end of year | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | $1,604,658 | $1,591,052 | $1,612,192 |
| Unobligated balance lapsing | -34 | 0 | 0 |
| Total obligations | $1,604,624 | $1,591,052 | $1,612,192 |
1 Excludes the following amounts for reimbursable activities carried out by this account: FY 2017 - $4,851 FY 2018 - $10,000 FY 2019 - $10,000
*Includes $57.500 million derived by transfer from the NIH Innovation Account
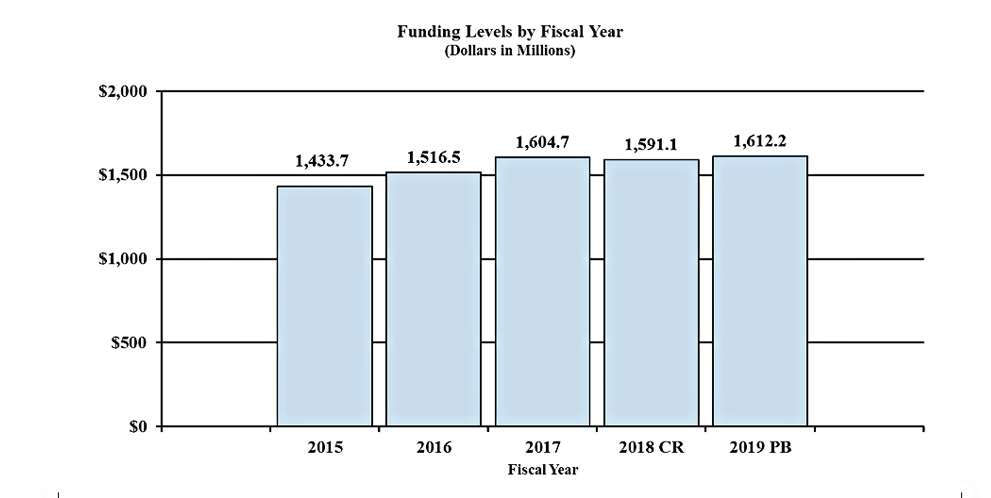
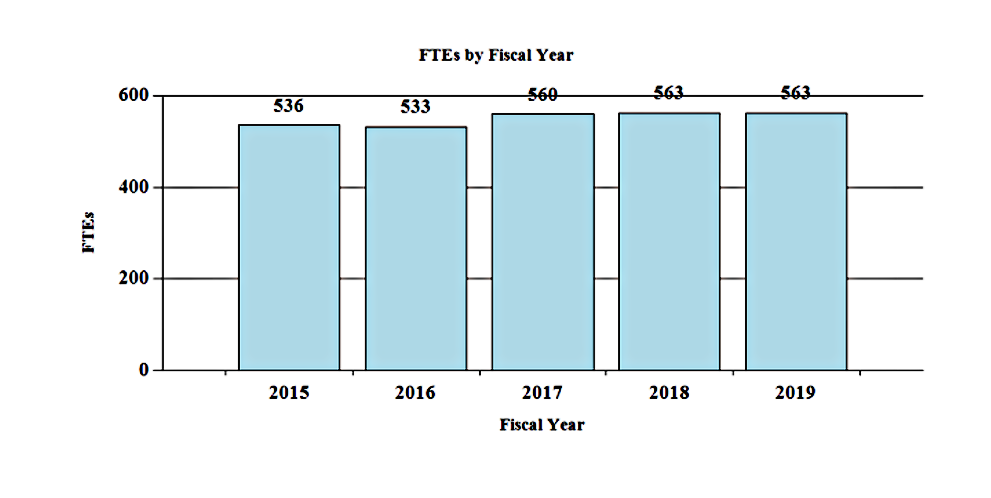
Fiscal Year 2019 Budget Graphs
History of Budget Authority and FTEs:
[Top]
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2018 Amount Authorized | FY 2018 Enacted | 2019 Amount Authorized | FY 2019
President's Budget |
|
|---|---|---|---|---|---|---|
| Research and Investigation | Section 301 | 42§241 | Indefinite | $1,591,052,287 | Indefinite | $1,612,192,000 |
| National Institute of Mental Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||
| Total, Budget Authority | $1,591,052,287 | $1,612,192,000 |
[Top]
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation |
|---|---|---|---|---|
| 2009 | $1,406,841,000 | $1,455,145,000 | $1,445,987,000 | $1,450,491,000 |
| Rescission | $0 | |||
| 2010 | $1,474,676,000 | $1,502,266,000 | $1,475,190,000 | $1,489,372,000 |
| Rescission | $0 | |||
| 2011 | $1,540,345,000 | $1,537,942,000 | $1,489,372,000 | |
| Rescission | $13,078,800 | |||
| 2012 | $1,517,006,000 | $1,517,006,000 | $1,460,671,000 | $1,483,068,000 |
| Rescission | $2,802,999 | |||
| 2013 | $1,479,204,000 | $1,483,687,000 | $1,480,265,001 | |
| Rescission | $2,960,530 | |||
| Sequestration | ($74,299,124) | |||
| 2014 | $1,465,782,000 | $1,456,041,000 | $1,446,172,000 | |
| Rescission | $0 | |||
| 2015 | $1,440,076,000 | 1,463,036,000 | ||
| Rescission | $0 | |||
| 2016 | $1,489,417,000 | $1,512,401,000 | $1,520,260,000 | $1,548,390,000 |
| Rescission | $0 | |||
| 2017[1] | $1,518,673,000 | $1,599,747,000 | $1,619,537,000 | $1,601,931,000 |
| Rescission | $0 | |||
| 2018 | $1,244,901,000 | $1,668,461,000 | $1,724,568,000 | $1,601,931,000 |
| Rescission | $10,878,713 | |||
| 2019 | $1,612,192,000 | $0 |
Justification of Budget Request
National Institute of Mental Health
Authorizing Legislation:
Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2017
Actual |
FY 2018
Annualized CR |
FY 2019
President's Budget |
FY 2019 +/- FY 2018 | |
|---|---|---|---|---|
| BA | $1,604,658,000 | $1,591,052,287 | $1,612,192,000 | $21,139,713 |
| FTE | 560 | 563 | 563 | 0 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements;
Contracts; Direct Federal/Intramural and Other.
Director’s Overview
The National Institute of Mental Health (NIMH) is the lead federal agency for research on mental illnesses, with a mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure. To optimize its scientific investments in the most rigorous research, NIMH follows its Strategic Plan for Research.1 The Institute supports basic, translational, clinical, and services research, including research with potential to improve clinical care over the short, medium, and long-term.
In the United States, an estimated 44.7 million adults suffer from a mental illness, which are significantly impairing and can be life-threatening.2 Mental and substance abuse disorders are the third leading cause of disability in the United States, accounting for 12.7 percent of all years lived with disability.3 One of the most tragic outcomes of untreated mental illness is suicide. Suicide accounts for the loss of more than 44,000 American lives each year; it is the second leading cause of death in youth and young adults aged 15-34, and the tenth leading cause of death overall.4
Tackling Complex Challenges by Leveraging Partnerships: Suicide prevention research is a top NIMH priority, and translating research findings into evidence-based practice requires strong collaborations. A member of the National Action Alliance for Suicide Prevention, NIMH supports the Alliance’s goal to reduce the U.S. suicide rate by 20 percent in 10 years.5 NIMH also works with the Substance Abuse and Mental Health Services Administration (SAMHSA) to implement two "practice ready" sets of tools: risk detection algorithms and risk reduction treatments. Past NIMH collaborations with the Army and the Department of Defense (DoD) produced screening tools and risk prediction algorithms. Current NIMH collaborations with the DoD, the Veterans Health Administration, and other agencies focus on suicide prevention in the military as one of many objectives. Additionally, NIMH intramural and extramural researchers developed suicide screening and intervention tools for use in multiple health care settings, such as emergency departments. With potential for near term impact, NIMH is also focused on the time course of suicide risk: in individuals identified as being at high risk, how long does this risk last? To answer this question, and to test and target interventions, NIMH and collaborators will facilitate data sharing as well as construction and use of registries and centralized data repositories (e.g., the NIMH Data Archive and the NIMH-funded Mental Health Research Network).6,7 These collaborative efforts aim to reverse the trend in rising suicide rates.
Supporting Basic Research: NIMH supports basic research through several mechanisms, including the NIH Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative.8 NIMH and the National Institute of Neurological Disorders and Stroke co-lead the BRAIN Initiative, which supports the development of new tools and technologies to revolutionize our understanding of the brain. NIMH led pilot projects aimed at classification strategies and data analyses for a comprehensive brain cell census.9 Based on this initial work, NIMH leads a coordinated set of awards under the auspices of the BRAIN Initiative Cell Census Network (BICCN).10 The BICCN aims to generate knowledge prerequisite to understanding brain disorders because relatively little is known about the different cell types and what they do—much less about how they change in illness. Evidence from a pilot phase points to potentially important roles in often overlooked cell types, such as support cells.11 Advances in neurotechnology aim to enhance knowledge about normal brain function and to improve methods for treating dysfunction. Because such advances carry potentially profound ethical implications, the NIH BRAIN Initiative Multi-Council Working Group created a Neuroethics Division of multidisciplinary experts to navigate unique ethical considerations associated with cutting-edge science the BRAIN Initiative supports.12
Investing in Translational and Clinical Research: NIMH leads the NIH Autism Coordinating Committee which supports research leading to identification of autism spectrum disorder (ASD) at the earliest age possible. Research demonstrates that ASD symptoms can begin to emerge as early as six months of age.13 NIMH supports research on early screening tools to identify children at risk for ASD before the emergence of full symptoms. NIMH funded the ASD Prevention, Early Detection, Engagement, and Services Research (PEDS) Network, which comprises five separate but coordinated studies to test a range of strategies for universal screening and early treatment.14 NIMH also aims to address research gaps on the risks and benefits of screening for ASD in young children.15 Screening children in primary care settings could help identify those at high risk for ASD, enabling early intervention and better long-term outcomes. Additional NIMH-funded efforts focus on improving accuracy of commonly used autism screening tools,16 developing and identifying early screening tools for vulnerable populations,17 and translating screening tools into clinical practice.18
Fostering a Diverse and Talented Workforce: NIMH supports highly talented students, postdoctoral fellows, and investigators from diverse backgrounds across a range of scientific opportunities. The NIMH Biobehavioral Research Awards for Innovative New Scientists (BRAINS) help exceptional early-career scientists launch innovative research programs that have potential to transform mental health research. NIMH administrative supplements support early-career individuals holding an M.D./Ph.D. degree to transition from clinical training to the next stage of their research careers.19 The NIMH Division of Intramural Research Programs provides diversity training opportunities for post-baccalaureate and postdoctoral fellows.20 As well, NIMH established the Collaborative Hubs for International Research on Mental Health program to support the mental health research workforce in low- and middle-income countries. 21,22
NIMH also supports NIH initiatives to foster a diverse and talented workforce. To address longstanding challenges faced by researchers trying to embark upon and sustain independent research careers, NIMH participates in the NIH Next Generation Researchers Initiative.23 and supports the development of Mentoring Networks for Health Research Education,24 and Research Education Mentoring for HIV AIDS Researchers,25 Additionally, NIMH participates in the NIH Blueprint Enhancing Neuroscience Diversity through Undergraduate Research Education Experiences (ENDURE) program which offers opportunities in neuroscience research for individuals from underrepresented racial and ethnic groups, individuals with disabilities, and those at economic disadvantage.26
Budget Policy: The FY 2019 President’s Budget estimate is $1,612.192 million, an increase of $21.140 million or 1.33 percent compared to the FY 2018 Annualized CR level.
Program Descriptions
Neuroscience and Basic Behavioral Science
The Division of Neuroscience and Basic Behavioral Science (DNBBS) provides support for research in the areas of basic neuroscience, genetics, basic behavioral science, research training, resource development, and drug discovery. In cooperation with other NIMH programs and the wider research community, this program ensures that relevant basic scientific knowledge is generated and used in pursuit of improved methods that, in the long term, could be used to diagnose, treat, and prevent mental illnesses.
DNBBS funds grants across a range of research topics to enhance understanding of the basic neurobiology underlying mental illnesses. In FY 2019, DNBBS plans to support research to determine if cognitive, affective, or social processing can be improved by modifying brain electrophysiological patterns. Cognitive, affective, and social processing can be disrupted in a variety of mental illnesses, and these efforts illustrate how basic research can provide a foundation for future treatment development.
Translational Research
The Division of Translational Research (DTR) supports integrative, multidisciplinary research and training programs that translate findings from basic science to discover the causes, mechanisms, and trajectories of mental illnesses, and develop effective interventions for individuals across the lifespan. DTR supports research on the characteristics of, and risk factors for, mental illnesses; the neurobehavioral mechanisms of psychopathology; the trajectories of risk and resilience based on the interactive influences of genetics, brain development, environment, and experience; and the design and testing of innovative treatments and interventions. As such, DTR-supported research efforts are designed to have intermediate-term impact.
One of DTR’s areas of high priority is to identify biological markers of risk/resilience and targets for intervention. To address this priority, NIMH recently funded a $20.6 million, five-year study to identify key factors in the development of mental illnesses that occur in the wake of trauma, how to better predict those outcomes, and to develop new targets for intervention.27 This landmark study, which will follow 5,000 participants over time, has the potential to define subtypes of post-traumatic stress based on objective neurobiological changes and other measures. In addition, through a collaboration with the National Institute on Aging, projects funded under the Adult Maturational Changes and Dysfunctions in Emotion Regulation initiative aims to advance the understanding of emotion processing in elderly individuals, and inform strategies that could prevent or ameliorate emotional dysfunction in later life.28 Ultimately, these initiatives could identify biological markers of risk/resilience and uncover new targets for interventions that could minimize potential adverse outcomes.
Services and Intervention Research
The Division of Services and Intervention Research (DSIR) supports research that evaluates the effectiveness of psychosocial, pharmacological, somatic, rehabilitative, and combined interventions to prevent or treat mental illnesses. DSIR refines and evaluates treatment and preventive interventions for children, adolescents, and adults, focusing on acute and long-term symptom reduction, remission, and improved community functioning. DSIR also supports mental health services research, including interventions to improve the quality and outcomes of care; organization- and system-level interventions to enhance service delivery; and strategies for widespread dissemination and implementation of evidence-based treatments into routine care settings. DSIR funds studies that are designed to have short-term impact, targeted at improving care for patients currently suffering from debilitating psychiatric disorders.
In FY 2017, DSIR supported large-scale initiatives to improve the effectiveness of mental health services delivered at critical periods of illness and across developmental life stages. Five grants examine suicide prevention practices in healthcare systems and juvenile justice settings, and test a range of interventions including: enhancing the identification of suicide risk factors and prevention using advanced information and communication technologies; linking suicide prevention practices across health care settings; and introducing decision aids into emergency departments to facilitate counseling. Another initiative focused on strategies for optimizing the independence and functioning of transition age youth and adults with autism spectrum disorder (ASD). Five grants test strategies for improving social, vocational, and physical health outcomes for persons with ASD across the lifespan.
Program Portrait: Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness (ALACRITY) Research Centers
In the United States, an estimated 44.7 million adults suffer from a mental illness.29 Mental illnesses often result in serious functional impairment, which substantially interferes with or limits one or more major life activities. To address this public health burden, NIMH issued a funding opportunity announcement in July, 2016 for Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness (ALACRITY) Research Centers.30 The goal of this effort is to improve the effectiveness, delivery, and quality of evidence-based services in diverse settings. ALACRITY Research Centers support transdisciplinary projects that could not be achieved using standard research project grant mechanisms. Projects may incorporate new discoveries in basic and clinical research, transformative health care technologies, advances in information science, behavioral economic strategies for influencing health behaviors, and new federal and state mechanisms for organizing and financing mental health care.
NIMH currently supports two ALACRITY Research Centers. The first Center is developing streamlined behavioral interventions based on input from consumers and community clinicians, guided by neurobiological models and big-data analytics, and supported by mobile technologies to improve the care of older and middle-aged adults with mood disorders.31 These novel interventions may be sustainably implemented in a variety of community settings and may reach populations for whom existing interventions or services do not adequately address urgent, unmet mental health needs. The second Center proposes a novel interdisciplinary approach at the intersection of behavioral economics and implementation science to drive improvements in the quality of evidence-based care and outcomes for persons with major depression, autism, or serious mental illness.32 The proposed projects capitalize on the multi-level nature of the treatment implementation process (e.g., patient, practitioner, and organization) and thus aim to develop and test strategies to improve treatment adherence among patients, treatment fidelity among providers, and practices among healthcare leaders to incentivize the delivery of evidence-based care within their systems.
Program Portrait: Suicide Prevention
Suicide prevention research is a top priority for NIMH. In 2015, suicide was the second leading cause of death in youth and young adults aged 15-34, and claimed the lives of more than 44,000 Americans across all ages.33 NIMH partners with the National Action Alliance for Suicide Prevention, supporting the “Zero Suicide” comprehensive research agenda aimed at reducing the U.S. suicide rate by 20 percent in 10 years.34 NIMH funds several Zero Suicide grants to create a stronger basis for dissemination and large-scale implementation of effective risk detection, intervention, and service delivery strategies for suicide prevention.35 Additional Zero Suicide efforts are underway to identify the most effective health care practice for reducing suicide risk in actual practice settings.36
Hospital emergency departments (EDs) can play a vital role in identifying suicide risk and decreasing suicide attempts among individuals, regardless of why they present in the ED. The Emergency Department Safety Assessment and Follow-up Evaluation (ED-SAFE) project demonstrated that ED-initiated interventions could reduce subsequent suicidal behavior among a sample of high-risk adult ED patients, with a decrease in suicide attempts by as much as 30 percent. A follow-on study, ED-SAFE-2, aims to examine both the sustainability of successfully implemented universal suicide risk screening and implementation of a brief suicide intervention.37 Additionally, the Emergency Department Screen for Teens at Risk for Suicide (ED-STARS) study generated a two minute, personally tailored, computerized screening tool for EDs to assess youth suicide risk.38 Researchers are examining adolescents from the ED-STARS cohort who are at immediate elevated risk for suicide to identify warning signs for suicide attempts.39
NIMH also supports suicide prevention research among vulnerable populations within specific communities. For example, collaborative research hubs aim to reduce the burden of suicide among urban American Indian and Alaska Native youth in both urban and rural settings.40 In addition, NIMH partners with the NIH Office of Behavioral Social Sciences Research and the National Institute of Justice to support a study to evaluate the effectiveness of an evidence-based safety planning intervention to reduce suicide events among persons recently released from incarceration.41
AIDS Research
The Division of AIDS Research (DAR) supports research and research training that addresses the priority areas outlined in the NIH HIV/AIDS Research Priorities and Guidelines for Determining AIDS Funding.42 DAR-supported research includes behavioral and social science studies aimed at reducing HIV/AIDS incidence through the development, testing, and implementation of new and improved prevention strategies, including expanded testing and linkage to care, vaccines, microbicides, and pre-exposure prophylaxis approaches. Behavioral and social science research is critical to understanding individual and community acceptance and uptake of prevention strategies, such that the delivery of these strategies is fully optimized, widely disseminated, and successfully implemented. Moreover, DAR research places special emphasis on World Health Organization-defined key populations, health disparities, and the impact of mental illnesses that may increase the risk for contracting HIV or negatively impact the health outcomes of those living with HIV.
DAR also supports research to understand, prevent, or treat the neurological dysfunction associated with HIV infection. DAR is participating in cure research by supporting studies to eradicate or silence the HIV virus from biological reservoirs in the central nervous system (CNS). HIV latency within the CNS is critically important to consider in studies of eradication and reactivation. Many drugs designed to eradicate the virus are unable to penetrate the CNS because it is a protected reservoir for HIV. This work may also inform methods to prevent or treat the neurological comorbidities of HIV, with targeted research to understand HIV-induced neurological pathology, with emphases on long-term antiretroviral therapy. Additionally, DAR ensures effective integration of biomedical approaches and multidisciplinary expertise are considered at agency-wide planning efforts, bringing us ever closer to an AIDS-free generation.
Intramural Research Programs
The Division of Intramural Research Programs (IRP) is the internal research component of NIMH, complementing the Institute’s extramural grant funding program. IRP scientists investigate basic, translational, and clinical aspects of brain function and behavior, conducting state-of-the-art research using unique NIH resources. In addition, the IRP provides an excellent environment for training the next generation of clinical and basic scientists.
IRP researchers continue to examine the relationship between genes, the brain, and behavior in healthy development and in adult- and childhood-onset mental illnesses. In FY 2017, many important scientific advances came out of the IRP, including: uncovering the molecular basis of premenstrual dysphoric disorder; leveraging a rare neuroimaging dataset to find effects of sex and sex chromosome complement on the structure of the cerebellum; and developing and sharing new research tools for controlling gene expression or analyzing brain images in animal models. IRP scientists investigate innovative behavioral treatments and medications for children with severe mood dysregulation or anxiety. They combine functional magnetic resonance imaging (fMRI) with transcranial magnetic stimulation to study brain connections involved in cognition. IRP researchers also explore novel medications for treatment-resistant depression in adults, including ketamine and other experimental fast-acting antidepressant medications, and work to understand the neurobiological underpinnings of suicide. In FY 2017, two new principal investigators joined the IRP whose research areas include combining technologies such as optogenetics – a method that uses light to manipulate living cells -- with neural recordings to study the brain circuits involved in making choices, and defining neural pathways involved in sleep, mood, and changes in circadian rhythms in response to environmental light/dark cycles.
Research Management and Support (RMS)
Research Management and Support (RMS) activities provide administrative, budgetary, logistical, and scientific support in the review, award, and monitoring of research and training grants, and research and development contracts. RMS functions include strategic planning, coordination, and evaluation of NIMH programs, regulatory compliance, coordination of global mental health efforts, and liaising with other Federal agencies, Congress, and the public. Through RMS activities, NIMH continues to provide administrative support for meritorious basic, clinical, and translational research and continues to promote health information dissemination and education/outreach activities.
1 http://www.nimh.nih.gov/about/strategic-planning-reports/index.shtml
2 SAMHSA. (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). Retrieved from https://www.samhsa.gov/data/
3 Institute of Health Metrics and Evaluation. http://ghdx.healthdata.org/gbd-results-tool accessed July 2017.
4 CDC, NCIPC. WISQARS: http://www.cdc.gov/injury/wisqars/index.html accessed October 2017.
5 http://actionallianceforsuicideprevention.org/sites/actionallianceforsuicideprevention.org/files/Agenda.pdf
6 https://data-archive.nimh.nih.gov/
7 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-14-110.html
8 https://braininitiative.nih.gov/
9 https://www.braininitiative.nih.gov/sites/default/files/pdfs/brain2025_508c.pdf
10 https://braininitiative.nih.gov/brain-programs/cell-census-network-biccn
11 https://www.ncbi.nlm.nih.gov/pubmed/28736215
12 https://www.braininitiative.nih.gov/about/neuroethics.htm
13 https://www.ncbi.nlm.nih.gov/pubmed/28592562
14 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-14-100.html
15 https://grants.nih.gov/grants/guide/notice-files/NOT-MH-18-001.html
16 https://reporter.nih.gov/project-details/9070770
17 https://reporter.nih.gov/project-details/9055759
18 https://reporter.nih.gov/project-details/9514336
19 https://grants.nih.gov/grants/guide/pa-files/PA-17-328.html
21 https://www.nimh.nih.gov/about/organization/gmh/globalhubs/index.shtml
22 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-17-350.html
23 https://grants.nih.gov/ngri.htm
24 https://grants.nih.gov/grants/guide/pa-files/PAR-17-080.html
25 https://grants.nih.gov/grants/guide/pa-files/PAR-17-485.html
26 https://neuroscienceblueprint.nih.gov/bp_nih-supported_training/endure_programs.htm
27 https://reporter.nih.gov/project-details/9174752
28 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-17-405.html
29 Substance Abuse and Mental Health Services Administration. (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). Retrieved from https://www.samhsa.gov/data/
30 https://grants.nih.gov/grants/guide/pa-files/PAR-16-354.html
31 https://reporter.nih.gov/project-details/9374695
32 https://reporter.nih.gov/project-details/9376070
33 CDC, NCIPC. WISQARS: http://www.cdc.gov/injury/wisqars/index.html accessed October 2017.
34 http://actionallianceforsuicideprevention.org/sites/actionallianceforsuicideprevention.org/files/Agenda.pdf
35 https://grants.nih.gov/grants/guide/rfa-files/rfa-mh-16-800.html
36 https://reporter.nih.gov/project-details/9380087
37 https://reporter.nih.gov/project-details/9234594
38 https://reporter.nih.gov/project-details/9142376
39 https://reporter.nih.gov/project-details/9363522
40 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-17-350.html
41 hhttps://reporter.nih.gov/project-details/9312313
42 https://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-137.html
[Top]
Detail of Full-Time Equivalent Employment (FTE)
| Office/Division | FY 2017
Final |
FY 2018
Annualized CR |
FY 2019
President's Budget |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of AIDS Research | |||||||||
| Direct: | 12 | - | 12 | 12 | - | 12 | 12 | - | 12 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 12 | - | 12 | 12 | - | 12 | 12 | - | 12 |
| Division of Extramural Activities | |||||||||
| Direct: | 43 | - | 43 | 43 | - | 43 | 43 | - | 43 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 43 | - | 43 | 43 | - | 43 | 43 | - | 43 |
| Division of Intramural Research Programs | |||||||||
| Direct: | 291 | - | 291 | 291 | - | 291 | 291 | - | 291 |
| Reimbursable: | 5 | - | 5 | 5 | - | 5 | 5 | - | 5 |
| Total: | 296 | - | 296 | 296 | - | 296 | 296 | - | 296 |
| Division of Neuroscience and Basic Behavioral Science | |||||||||
| Direct: | 22 | - | 22 | 22 | - | 22 | 22 | - | 22 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 22 | - | 22 | 22 | - | 22 | 22 | - | 22 |
| Division of Services and Intervention Branch | |||||||||
| Direct: | 12 | 1 | 13 | 13 | - | 13 | 13 | - | 13 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 12 | 1 | 13 | 13 | - | 13 | 13 | - | 13 |
| Division of Translational Research | |||||||||
| Direct: | 24 | - | 24 | 24 | - | 24 | 24 | - | 24 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 24 | - | 24 | 24 | - | 24 | 24 | - | 24 |
| Office of the Director | |||||||||
| Direct: | 141 | - | 141 | 144 | - | 144 | 144 | - | 144 |
| Reimbursable: | 9 | - | 9 | 9 | - | 9 | 9 | - | 9 |
| Total: | 150 | - | 150 | 153 | - | 153 | 153 | - | 153 |
| Total | 559 | 1 | 560 | 563 | - | 563 | 563 | - | 563 |
Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
| Office/Division | FY 2017
Final |
FY 2018
Annualized CR |
FY 2019
President's Budget |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| FTEs supported by funds from Cooperative Research and Development Agreements. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fiscal Year | Average GS Grade |
|---|---|
| 2015 | 12.7 |
| 2016 | 12.4 |
| 2017 | 12.6 |
| 2018 | 12.6 |
| 2019 | 12.6 |
[Top]
Detail of Positions [1]
| Grade | FY 2017
Final |
FY 2018
Annualized CR |
FY 2019
President's Budget |
|---|---|---|---|
| Total, ES Positions | 1 | 1 | 1 |
| Total, ES Salary | 168,400 | 168,400 | 168,400 |
| GM/GS-15 | 61 | 61 | 61 |
| GM/GS-14 | 70 | 70 | 70 |
| GM/GS-13 | 110 | 113 | 113 |
| GS-12 | 70 | 70 | 70 |
| GS-11 | 53 | 53 | 53 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 19 | 19 | 19 |
| GS-8 | 9 | 9 | 9 |
| GS-7 | 7 | 7 | 7 |
| GS-6 | 1 | 1 | 1 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 2 | 2 | 2 |
| GS-3 | 1 | 1 | 1 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 403 | 406 | 406 |
| Grades established by Act of July 1, 1944 (42 U.S.C. 207): | 0 | 0 | 0 |
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 1 | 0 | 0 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 1 | 0 | 0 |
| Ungraded | 179 | 179 | 179 |
| Total permanent positions | 406 | 406 | 406 |
| Total positions, end of year | 584 | 584 | 584 |
| Total full-time equivalent (FTE) employment, end of year | 560 | 563 | 563 |
| Average ES salary | 168,400 | 168,400 | 168,400 |
| Average GM/GS grade | 12.6 | 12.6 | 12.6 |
| Average GM/GS salary | 110,319 | 112,470 | 113,004 |
