FY 2018 Budget — Congressional Justification
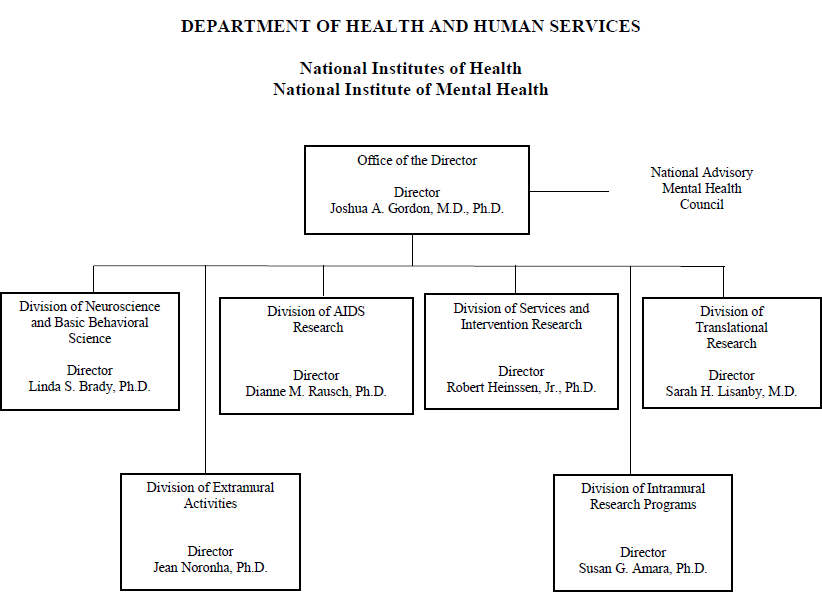
- Organization Chart
- Appropriation Language
- Amounts Available for Obligation
- Budget Graphs
- Authorizing Legislation
- Appropriations History
- Justification of Budget Request
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
Department of Health and Human Services
National Institutes of Health
National Institute of Mental Health
Organization Chart
[Top]
Appropriation Language
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
For carrying out section 301 and title IV of the PHS Act with respect to mental health, $1,201,901,000.
[Top]
Amounts Available for Obligation
| Source of Funding | FY 2016
Final |
FY 2017
Annualized CR |
FY 2018
President's Budget* |
|---|---|---|---|
| Appropriation | $1,548,390 | $1,548,390 | $1,244,901 |
| Mandatory Appropriation (non-add) | |||
| Type 1 Diabetes | (0) | (0) | (0) |
| Other Mandatory financing | (0) | (0) | (0) |
| Rescission | 0 | -2,943 | 0 |
| Sequestration | 0 | 0 | 0 |
| Zika Intra-NIH Transfer | -2,143 | 0 | 0 |
| Subtotal, adjusted appropriation | $1,546,247 | $1,545,447 | $1,244,901 |
| OAR HIV/AIDS Transfers | -29,717 | 0 | 0 |
| Subtotal, adjusted budget authority | $1,516,530 | $1,545,447 | $1,244,901 |
| Unobligated balance, start of year | 0 | 0 | 0 |
| Unobligated balance, end of year | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | $1,516,530 | $1,545,447 | $1,244,901 |
| Unobligated balance lapsing | -205 | 0 | 0 |
| Total obligations | $1,516,325 | $1,545,447 | $1,244,901 |
1 Excludes the following amounts for reimbursable activities carried out by this account: FY 2016 - $6,223 FY 2017 - $10,050 FY 2018 - $10,050
*Of which $43,000,000 is derived by transfer from the NIH Innovation Account.
[Top]
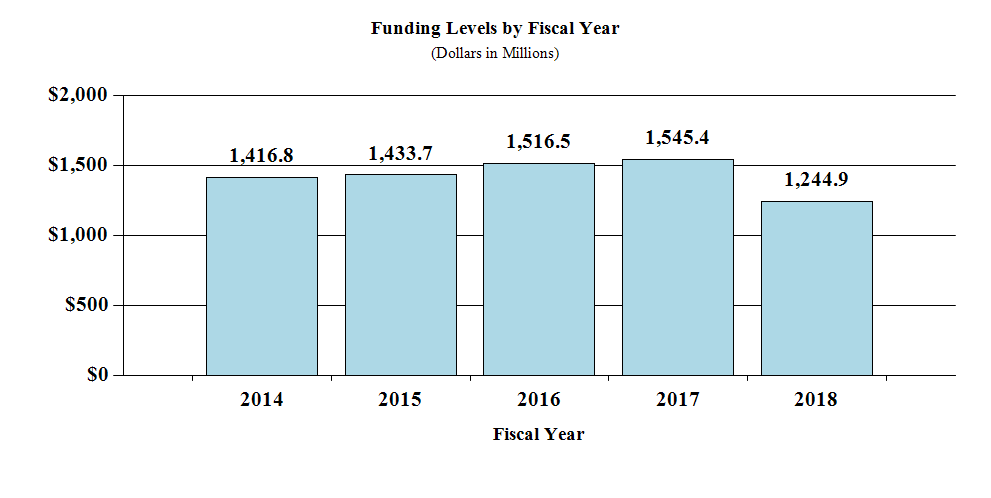
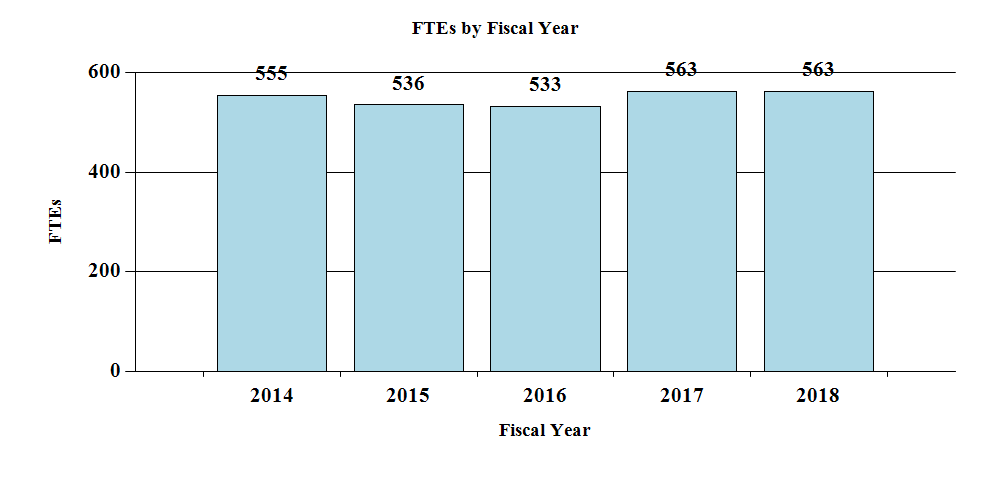
Budget Graphs
History of Budget Authority and FTEs:
[Top]
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2017 Amount Authorized | FY 2017 Enacted | 2018 Amount Authorized | FY 2018
President's Budget |
|
|---|---|---|---|---|---|---|
| Research and Investigation | Section 301 | 42§241 | Indefinite | $1,545,447,000 | Indefinite | $1,244,901,000 |
| National Institute of Mental Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||
| Total, Budget Authority | $1,545,447,000 | $1,244,901,000 |
[Top]
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation |
|---|---|---|---|---|
| 2008 | $1,405,421,000 | $1,425,531,000 | $1,436,001,000 | $1,429,466,000 |
| Rescission | $24,973,000 | |||
| Supplemental | $7,475,000 | |||
| 2009 | $1,406,841,000 | $1,455,145,000 | $1,445,987,000 | $1,450,491,000 |
| Rescission | $0 | |||
| 2010 | $1,474,676,000 | $1,502,266,000 | $1,475,190,000 | $1,489,372,000 |
| Rescission | $0 | |||
| 2011 | $1,540,345,000 | $1,537,942,000 | $1,489,372,000 | |
| Rescission | $13,078,800 | |||
| 2012 | $1,517,006,000 | $1,517,006,000 | $1,460,671,000 | $1,483,068,000 |
| Rescission | $2,802,999 | |||
| 2013 | $1,479,204,000 | $1,483,687,000 | $1,480,265,001 | |
| Rescission | $2,960,530 | |||
| Sequestration | ($74,299,124) | |||
| 2014 | $1,465,782,000 | $1,456,041,000 | $1,446,172,000 | |
| Rescission | $0 | |||
| 2015 | $1,440,076,000 | 1,463,036,000 | ||
| Rescission | $0 | |||
| 2016 | $1,489,417,000 | $1,512,401,000 | $1,520,260,000 | $1,548,390,000 |
| Rescission | $0 | |||
| 2017[1] | $1,518,673,000 | $1,599,747,000 | $1,619,537,000 | $1,548,390,000 |
| Rescission | $2,943,000 | |||
| 2018 | $1,244,901,000 |
[Top]
Justification of Budget Request
Authorizing Legislation:
Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2016
Actual |
FY 2017
CR Annualized |
FY 2018
President's Budget |
FY 2018 +/- FY 2017 | |
|---|---|---|---|---|
| BA | $1,516,530,000 | $1,545,447,000 | $1,244,901,000 | -$300,546,000 |
| FTE | 533 | 563 | 563 | 0 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements;
Contracts; Direct Federal/Intramural and Other.
Director’s Overview
The National Institute of Mental Health (NIMH) is the lead Federal agency for research on mental illnesses, with a mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure.
In the United States, an estimated 43.4 million adults suffer from a mental illness.1 Mental illnesses are significantly impairing and can be life-threatening. Based on the most recent estimates, mental illnesses accounted for 21.3 percent of all years lived with disability in the United States.2 Suicide accounts for the loss of more than 42,000 American lives each year; it is the second leading cause of death in youth and young adults aged 10-34, and the tenth leading cause of death overall in the United States.3
On September 12, 2016, NIMH welcomed new Director, Joshua A. Gordon, M.D., Ph.D. Dr. Gordon’s experience as both a clinician and basic science researcher will serve NIMH well as he oversees a diverse portfolio of basic, translational, and clinical research, including investments in research with short-, medium-, and long-term outcomes. To optimize its scientific investments in the most rigorous research, NIMH is guided by its Strategic Plan for Research.4
Fundamental Science: Many important medical advances trace back to basic research. For example, NIMH scientists and collaborators recently uncovered the mechanisms behind the rapid antidepressant effects of ketamine, an anesthetic drug, in individuals with treatment-resistant depression. Results revealed that a byproduct of ketamine’s chemical breakdown, and not ketamine itself, produces the antidepressant effects. Identifying this mechanism is a crucial step in the drug development process, and highlights the importance of basic science in getting treatments to patients.
NIMH plays a key role in the NIH Human Connectome Project (HCP), which aims to map the neural pathways that underlie human brain function. In the first phase of the HCP, researchers identified more than twice the previously known number of human brain regions, and demonstrated that individual differences in brain connectivity can predict performance on a variety of tasks.5, 6, 7 NIMH also plays a leading role in the NIH Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative, which aims to revolutionize our understanding of the human brain by accelerating the development and application of innovative technologies. NIMH-funded BRAIN Initiative researchers identified new methods for classifying neuron types, and discovered several genetic mechanisms in brain cells.8, 9 NIH recently announced its third round of BRAIN Initiative grants; NIMH will support a variety of projects including novel methods to better understand brain cells and circuits, and new approaches to noninvasive brain-based treatments for mental illnesses. The HCP and the BRAIN Initiative support studies that demonstrate novel methods and findings that may prove important for uncovering neuronal dysfunction in mental illnesses.
Treatments and Cures: NIMH supports research for treatments and cures for mental disorders, spanning novel intervention development, efficacy testing, and effectiveness testing in community practice settings. Approximately 50 percent of NIMH’s budget is dedicated to clinical research. NIMH currently devotes nearly 10 percent of its budget to clinical trials. One such clinical trial is the Prolonging Remission in Depressed Elderly (PRIDE) study, which demonstrated that electroconvulsive therapy (ECT) combined with an antidepressant prevented relapse in patients 60 years and older suffering from severe depression.10, 11 NIMH is also investing in technology to screen rapidly for small but meaningful biological indicators, or biomarkers. For example, the Autism Biomarkers Consortium for Clinical Trials aims to develop biomarkers to identify biological subtypes of autism spectrum disorder (ASD) and predict the best treatment options for individuals with ASD. NIMH also recently issued a funding opportunity announcement for Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness (ALACRITY) Research Centers.12 The goal of this effort is to improve the effectiveness, delivery, and quality of evidence-based services in diverse settings.
Health Promotion and Disease Prevention: NIMH supports efforts to identify genetic and environmental risk factors for suicide, develop strategies to reduce suicide, and promote mental health. As a member of the National Action Alliance for Suicide Prevention, NIMH supports the Alliance’s Zero Suicide commitment to reduce suicide, and to identify and implement effective treatments for at-risk individuals.13 NIMH recently funded three Zero Suicide studies focused on adult and youth based suicide prevention practices in health care settings. These efforts include improving the quality of behavioral health care to reduce suicide risk, testing the efficacy of a suicide prevention approach, and identifying youth at risk for suicidal behavior. Other NIMH-funded suicide prevention efforts focus on vulnerable populations including teens, individuals transitioning from jail to community settings, and arctic indigenous peoples.
Enhancing Stewardship: NIMH is increasing transparency and accountability through data sharing and oversight. NIMH strongly encourages investigators to use common data elements and share data through databases and repositories, such as the NIMH Data Archive.14 In June 2016, NIMH hosted a webinar to encourage scientists to confirm research findings and to use existing data to answer research questions in a cost-effective way. NIMH is also improving oversight and monitoring of clinical trials. For example, in 2016, NIMH expanded the Policy for the Recruitment of Participants in Clinical Research15 to apply to all clinical trials, regardless of size, to ensure studies are meeting their recruitment goals.16 NIMH also implemented the Proactive Site Monitoring Program and increased its ClinicalTrials.gov registration rate to 97 percent, improving oversight and public access to clinical trials information.
NIMH places a high priority on supporting outstanding scientists who will advance the field to help people with mental illnesses. In May 2016, four NIMH-supported early stage investigators received the Presidential Early Career Award for Scientists and Engineers (PECASE). NIMH is also committed to improving recruitment and retention of early stage investigators from underrepresented groups, and offers administrative supplements for individuals from diverse backgrounds.17, 18, 19
Overall Budget Policy:
The FY 2018 President’s Budget request is $1,244.901 million, a decrease of $300.546 million compared with the FY 2017 Annualized CR level. These reductions are distributed across all programmatic areas and basic, epidemiology, or clinical research.
Program Descriptions
Neuroscience and Basic Behavioral Science
The Division of Neuroscience and Basic Behavioral Science (DNBBS) supports research in the areas of basic neuroscience, genetics, basic behavioral science, research training, resource development, and drug discovery. In cooperation with other NIMH programs and the wider research community, DNBBS ensures that relevant basic scientific knowledge is generated and used in pursuit of improved methods that, in the long term, will be used to diagnose, treat, and prevent mental illnesses.
DNBBS funds grants across a range of research topics to enhance our comprehension of the basic neurobiology underlying mental illnesses. In FY 2018, DNBBS will continue to build on strengths in neuroscience research into the brain mechanisms underlying social interactions. In particular, DNBBS will support research into social interactions that involve multiple social modalities and the brain circuits underlying those interactions, either positive or negative. For example, disorders such as ASD and schizophrenia are marked by disrupted social interactions and responses to social cues. By fostering research into these areas, DNBBS intends to open up new possibilities for treatment development and disease prevention.
Translational Research
The Division of Translational Research (DTR) supports integrative, multidisciplinary research, and training programs that translate findings from basic science in order to discover the causes, mechanisms, and trajectories of mental illnesses, and to develop effective interventions for children and adults. DTR supports research on the characteristics of and risk factors for mental illnesses; the neurobehavioral mechanisms of psychopathology; the trajectories of risk and resilience based on the interactive influences of genetics, brain development, environment, and experience; and, the design and testing of innovative treatments and interventions. As such, DTR-supported research efforts are designed to have predominantly medium-term impact.
Despite the existence of promising technology-based interventions, few tools are being adapted to advance social functioning for individuals with social deficits. In FY 2017, NIMH will launch projects funded under the Adaptation/Optimization of Technology (ADOPTech) to Support Social Functioning initiative to develop and test cutting edge technologies to enhance social functioning in individuals with mental illnesses.20 This effort also aims to stimulate collaboration between clinical scientists and their colleagues in engineering, mathematics, physics, and computer science. Projects funded under this program may create “social prosthetics,” or high-tech devices that could dramatically improve social skills and the quality of life for people with mental illnesses. Prior research indicates that emotion regulation improves with aging. Yet, a major gap remains with regard to how these maturational changes confer risk or resilience to emotional problems seen in mental disorders that arise in later adulthood. In FY 2016, in collaboration with the National Institute on Aging, DTR issued a joint initiative entitled Adult Maturational Changes and Dysfunctions in Emotion Regulation.21 Projects funded under this initiative will begin in 2017 and will advance our understanding of emotion processing in the elderly, and inform strategies that could prevent or ameliorate emotional dysfunction in later life. Ultimately, these projects could uncover new targets for interventions that could minimize emotion dysregulation or preventively build resilience in aging adults.
Services and Intervention Research
The Division of Services and Intervention Research (DSIR) supports research that evaluates the effectiveness of psychosocial, pharmacological, somatic, rehabilitative, and combined interventions to prevent or treat mental and behavioral illnesses. DSIR refines and evaluates treatment and preventive interventions for children, adolescents, and adults, focusing on acute and long-term symptom reduction, remission, and improved community functioning. DSIR also supports mental health services research, including interventions to improve the quality and outcomes of care; organization- and system-level interventions to enhance service delivery; and, strategies for widespread dissemination and implementation of evidence-based treatments into routine care settings. Studies funded by DSIR are designed to have short-term impact, targeted at improving care for patients currently suffering from debilitating psychiatric disorders.
In FY 2016, DSIR supported large-scale initiatives to improve the effectiveness of mental health services delivered at critical periods of illness and across developmental life stages. Three grants funded in FY 2016 examine suicide prevention practices in healthcare systems, and test a range of interventions including: enhancing suicide prevention in a state-wide behavioral health system using quality improvement methods; linking suicide prevention practices across health care settings; and, matching suicidal youths’ level of risk to the intensity of care. Another project tests treatment for youth with behavioral and emotional problems, and beginning with psychosocial intervention, progressing to non-antipsychotic medications if required, and introducing targeted antipsychotic pharmacotherapy if needed. Three other grants test a variety of intervention models for reducing weight gain and cardio-metabolic risk among youth receiving antipsychotic medications. These intervention models include a parent-delivered healthy lifestyle intervention, weight management counseling to reduce cardiovascular risk factors, and a group-based intervention supported by mobile health technology.
Program Portrait: Reducing the Duration of Untreated Psychosis
| FY 2017 Level: | $8.3 million |
|---|---|
| FY 2018 Level: | $6.7 million |
| Change: | -$1.6 million |
Each year approximately 100,000 adolescents and young adults in the United States experience a first episode of psychosis (FEP).22 The beginning of the acute phase of psychotic illness is a critical opportunity for prevention, and a chance to alter the downward trajectory and poor outcomes associated with psychotic disorders. The timing of treatment is critical; short- and long-term outcomes are better when individuals begin treatment close to the onset of psychosis.23 Unfortunately, numerous studies find a substantial delay between onset of FEP and the initiation of care.24 In one NIMH-funded study, psychosis treatment was delayed a median of 74 weeks for patients seen in 34 U.S. community clinics.25
A major focus of NIMH’s applied research efforts is the identification of screening and referral strategies that could reduce the duration of untreated psychosis in the United States from the current average of 1-3 years to the international standard of no more than three months.26 Research to improve FEP case identification and referral to treatment complements other NIMH initiatives, such as the Recovery After an Initial Schizophrenia Episode (RAISE) project, that aimed to improve outcomes for people experiencing FEP. Recent findings from the RAISE project indicate that coordinated specialty care (CSC) - a team-based, multi-component treatment program for FEP - produced superior clinical and functional improvements compared to typical care, especially among clients with shorter duration of untreated psychosis.27
To build on the successes of RAISE, in May 2016, NIMH reissued funding opportunity announcements seeking projects aiming to reduce the duration of untreated psychosis.28 Specifically, NIMH aims to support research that tests practical, reproducible strategies for substantially reducing the duration of psychosis among persons with FEP by eliminating bottlenecks or closing gaps in the pathway to CSC services. NIMH currently funds eight such studies aiming to reduce the duration of untreated psychosis. Early identification of FEP, rapid referral to evidence-based services, and effective engagement in CSC are essential to shortening the duration of untreated psychosis, pre-empting the functional deterioration common in psychotic disorders, and reducing the economic burden of these devastating illnesses on society.
The decrease in funding in FY 2018 for this program will bring commitments in line with available resources.
Program Portrait: Identifying Key Factors and Novel Targets in Post-Traumatic Stress Disorders
| FY 2017 Level: | $43.3 million |
|---|---|
| FY 2018 Level: | $34.7 million |
| Change: | -$8.6 million |
Following any traumatic event, it is common for people to report a range of symptoms including hypervigilance, intrusive upsetting thoughts, flashbacks, and changes in sleep and mood. Although most people gradually recover, some develop persistent problems, and may be diagnosed with post-traumatic stress disorder (PTSD).
In 2012, the Departments of Health and Human Services (including NIH), Defense, Veterans Affairs, and Education developed the National Research Action Plan (NRAP). The NRAP is designed to accelerate discovery of the causes and mechanisms underlying PTSD, other conditions, and their co-occurring outcomes like suicide, depression, and substance abuse disorders. Consistent with the NRAP, NIMH recently funded a $21 million, five-year study to identify key factors in the development of mental disorders that occur in the wake of trauma, better predict those outcomes, and develop new targets for intervention.29 This landmark study, which will follow 5,000 people over time, has the potential to define subtypes of post-traumatic stress based on objective neurobiological changes and other measures. Such efforts have the potential improve the care of individuals at high risk for post-traumatic stress conditions across civilian, military, and veteran populations.
NIMH recognizes the urgent need to improve therapies for post-traumatic stress conditions, and supports a diverse research portfolio on PTSD. For example, researchers are studying a novel medication that may reduce hyperarousal and fear generalization; and separately, a drug used to treat other diseases that may help eliminate fear responses in individuals with PTSD.30, 31 Because sleep abnormalities are common in PTSD, other NIMH-funded researchers are treating insomnia to determine if less fragmented sleep leads to better emotion regulation in PTSD.32 To improve treatments that directly treat brain circuit abnormalities, some researchers are combining noninvasive brain stimulation and imaging to create personalized maps that show cause and effect of the stimulation, allowing greater precision and tailored neuromodulatory treatments.33 NIMH’s commitment to PTSD research is designed to lead to better understanding and improved treatments for post-traumatic stress conditions.
The decrease in funding in FY 2018 for this program will bring commitments in line with available resources.
AIDS Research
The Division of AIDS Research (DAR) supports research and research training addressing the priority areas outlined in the NIH HIV/AIDS Research Priorities and Guidelines for Determining AIDS Funding.34 DAR supports behavioral and social science research critical to the goal of reducing HIV/AIDS incidence through developing and testing new prevention strategies, including expanded testing and linkage to care, vaccines, microbicides, and pre-exposure prophylaxis approaches. Behavioral and social science research is critical to understanding individual and community acceptance of prevention strategies, so that the delivery of such strategies is fully optimized, widely disseminated, and successfully implemented. Moreover, DAR research places special emphasis on World Health Organization-defined key populations, health disparities, and the impact of mental illnesses that may increase the risk for HIV acquisition or negatively impact the health outcomes of those living with HIV.
DAR is also actively participating in cure efforts by supporting research on methods to eliminate HIV in infected individuals by eradicating or silencing the virus from biological reservoirs in the central nervous system (CNS). As many drugs designed to eradicate the virus are unable to penetrate the CNS, the CNS can act as a protected reservoir for HIV. Therefore, HIV latency within the CNS is critically important to consider in studies of eradication and reactivation. This work may also inform methods to prevent or treat the neurological comorbidities of HIV, with targeted research to understand HIV-induced neurological pathology, with a particular emphasis on the premature aging associated with long-term HIV disease and long-term antiretroviral therapy. Through its commitment to bringing multidisciplinary expertise to agency-wide strategic planning efforts, DAR is working to ensure that effective integration of biomedical and behavioral approaches is accomplished, bringing us ever closer to an AIDS-free generation.
Intramural Research Programs
The Division of Intramural Research Programs (IRP) is the internal research component of NIMH, complementing the Institute’s extramural grant funding program. IRP scientists investigate basic, translational, and clinical aspects of brain function and behavior, conducting state-of-the-art research through the use of unique NIH resources. In addition, the IRP provides an excellent environment for training the next generation of clinical and basic scientists.
IRP researchers continue to examine the relationship between genes, the brain, and behavior in healthy development and in adult- and childhood-onset mental illnesses. In FY 2016, many important science advances came out of the IRP, including: identifying genomic risk factors for bipolar disorder and schizophrenia; linking specific patterns of brain activity, called ‘euronal avalanches,’ to changes in physiological state; and, using chemogenetic designer-receptor-exclusively-activated-by-designer-drug (DREADD) technology to study brain circuits involved in cognition. IRP scientists use functional magnetic resonance imaging (fMRI) to study brain connectivity among networks implicated in ASD, and they investigate innovative behavioral treatments for children with severe mood dysregulation or anxiety. IRP researchers also explore novel medications for treatment-resistant depression in adults including ketamine and other experimental fast-acting antidepressant medications, and work to identify biomarkers for predicting how well an individual with depression will respond to such rapid-acting antidepressants. In FY 2016, four new tenure-track scientists joined the IRP whose research areas include: the effect of stress on memory and behavior; cortical circuits and activity patterns linked to behavioral decision-making; top-down modulation of sensory processes; and, mood disorders in young people.
Research Management and Support (RMS)
RMS provides leadership to NIMH, as well as administrative, budgetary, logistical, and scientific support in the review, award, and monitoring of research grants, training grants, and research and development contracts. RMS functions include strategic planning, coordination, and evaluation of NIMH programs; regulatory compliance; coordinating global mental health efforts; and, liaising with other Federal agencies, Congress, and the public. In FY 2016 NIMH managed 2,481 research grants, 307 training grants that supported 705 full-time trainee positions, and 200 research and development contracts.
1 Center for Behavioral Health Statistics and Quality. (2016). Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. (HHS Publication No. SMA, NSDUH Series H-51). Retrieved from http://www.samhsa.gov/data
2 US Burden of Disease Collaborators. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA, 310(6): 591-608, 2013.
3 CDC, NCIPC. WISQARS: http://www.cdc.gov/injury/wisqars/index.html accessed October 2016.
4 https://www.nimh.nih.gov/about/strategic-planning-reports/index.shtml
5 https://www.ncbi.nlm.nih.gov/pubmed/27437579
6 https://www.ncbi.nlm.nih.gov/pubmed/26457551
7 https://www.ncbi.nlm.nih.gov/pubmed/27124457
8 https://www.ncbi.nlm.nih.gov/pubmed/27565351
9 https://www.ncbi.nlm.nih.gov/pubmed/27113499
10 https://www.ncbi.nlm.nih.gov/pubmed/27418379
11 https://www.ncbi.nlm.nih.gov/pubmed/27418381
12 http://grants.nih.gov/grants/guide/pa-files/PAR-16-354.html
13 http://zerosuicide.sprc.org/
14 http://data-archive.nimh.nih.gov/
15 See https://www.nimh.nih.gov/funding/grant-writing-and-application-process/nimh-policy-for-the-recruitment-of-participants-in-clinical-research.shtml
17 http://grants.nih.gov/grants/guide/pa-files/PA-16-288.html
18 http://grants.nih.gov/grants/guide/pa-files/PA-14-263.html
19 http://grants.nih.gov/grants/guide/pa-files/PA-15-069.html
20 http://grants.nih.gov/grants/guide/rfa-files/RFA-MH-17-150.html
21 http://grants.nih.gov/grants/guide/rfa-files/RFA-MH-17-405.html
22 https://www.ncbi.nlm.nih.gov/pubmed/22457710
23 https://www.ncbi.nlm.nih.gov/pubmed/26481174
24 https://www.ncbi.nlm.nih.gov/pubmed/16143729
25 https://www.ncbi.nlm.nih.gov/pubmed/25588418
26 https://www.ncbi.nlm.nih.gov/pubmed/16055800
27 https://www.ncbi.nlm.nih.gov/pubmed/26481174
28 http://grants.nih.gov/grants/guide/pa-files/PAR-16-265.html
29 https://reporter.nih.gov/project-details/9174752
30 https://reporter.nih.gov/project-details/9164410
31 https://reporter.nih.gov/project-details/9017400
32 https://reporter.nih.gov/project-details/9325818
33 https://reporter.nih.gov/project-details/9109051
34 See https://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-137.html
[Top]
Detail of Full-Time Equivalent Employment (FTE)
| Office/Division | FY 2016
Final |
FY 2017
Annualized CR |
FY 2018
President's Budget |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of AIDS Research | |||||||||
| Direct: | 12 | - | 12 | 12 | - | 12 | 12 | - | 12 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 12 | - | 12 | 12 | - | 12 | 12 | - | 12 |
| Division of Extramural Activities | |||||||||
| Direct: | 41 | - | 41 | 42 | - | 42 | 42 | - | 42 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 41 | - | 41 | 42 | - | 42 | 42 | - | 42 |
| Division of Intramural Research Programs | |||||||||
| Direct: | 274 | 1 | 275 | 298 | 1 | 299 | 298 | 1 | 299 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 274 | 1 | 275 | 298 | 1 | 299 | 298 | 1 | 299 |
| Division of Neuroscience and Basic Behavioral Science | |||||||||
| Direct: | 22 | - | 22 | 22 | - | 22 | 22 | - | 22 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 22 | - | 22 | 22 | - | 22 | 22 | - | 22 |
| Division of Services and Intervention Branch | |||||||||
| Direct: | 15 | 1 | 16 | 12 | 1 | 13 | 12 | 1 | 13 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 15 | 1 | 16 | 12 | 1 | 13 | 12 | 1 | 13 |
| Division of Translational Research | |||||||||
| Direct: | 28 | - | 28 | 23 | - | 23 | 23 | - | 23 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 28 | - | 28 | 23 | - | 23 | 23 | - | 23 |
| Office of the Director | |||||||||
| Direct: | 139 | - | 139 | 152 | - | 152 | 152 | - | 152 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 139 | - | 139 | 152 | - | 152 | 152 | - | 152 |
| Total | 531 | 2 | 533 | 561 | 2 | 563 | 561 | 2 | 563 |
Includes FTEs whose payroll obligations are supported by NIH Common Fund.
| Office/Division | FY 2016
Final |
FY 2017
Annualized CR |
FY 2018
President's Budget |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| FTEs supported by funds from Cooperative Research and Development Agreements. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fiscal Year | Average GM/GS Grade |
|---|---|
| 2014 | 12.3 |
| 2015 | 12.7 |
| 2016 | 12.4 |
| 2017 | 12.4 |
| 2018 | 12.4 |
[Top]
Detail of Positions [1]
| Grade | FY 2016
Final |
FY 2017
Annualized CR |
FY 2018
President's Budget |
|---|---|---|---|
| Total, ES Positions | 1 | 1 | 1 |
| Total, ES Salary | 158,868 | 168,400 | 168,400 |
| GM/GS-15 | 62 | 61 | 61 |
| GM/GS-14 | 63 | 68 | 68 |
| GM/GS-13 | 100 | 109 | 109 |
| GS-12 | 62 | 69 | 69 |
| GS-11 | 53 | 59 | 59 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 25 | 22 | 22 |
| GS-8 | 11 | 9 | 9 |
| GS-7 | 8 | 7 | 7 |
| GS-6 | 1 | 1 | 1 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 0 | 0 | 0 |
| GS-3 | 1 | 1 | 1 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 386 | 406 | 406 |
| Grades established by Act of July 1, 1944 (42 U.S.C. 207): | 0 | 0 | 0 |
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 2 | 2 | 2 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 2 | 2 | 2 |
| Ungraded | 157 | 190 | 190 |
| Total permanent positions | 390 | 410 | 410 |
| Total positions, end of year | 546 | 598 | 598 |
| Total full-time equivalent (FTE) employment, end of year | 533 | 563 | 563 |
| Average ES salary | 158,868 | 168,400 | 168,400 |
| Average GM/GS grade | 12.4 | 12.4 | 12.4 |
| Average GM/GS salary | 106,894 | 109,139 | 111,213 |
