FY 2017 Budget - Congressional Justification
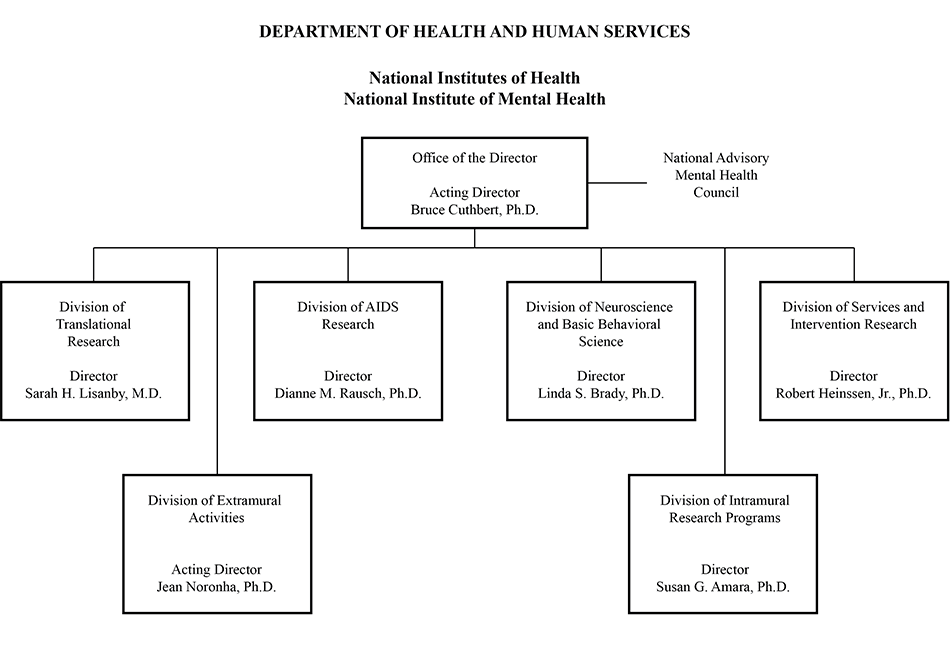
- Organization Chart
- Appropriation Language
- Amounts Available for Obligation
- Budget Mechanism Table
- Major Changes in Budget Request
- Summary of Changes
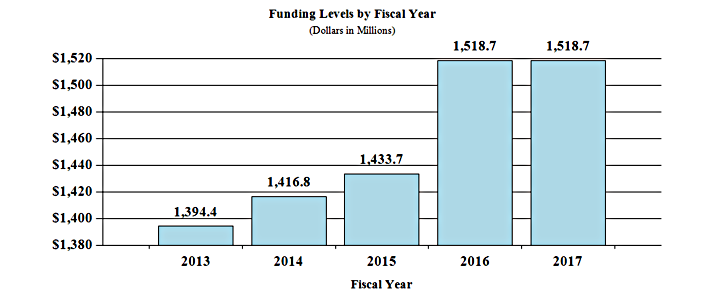
- Budget Graphs
- Budget Authority by Activity
- Authorizing Legislation
- Appropriations History
- Justification of Budget Request
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
Note: The FY 2016 Enacted funding amounts cited throughout this chapter reflect the effects of OAR HIV/AIDS Transfers.
Department of Health and Human Services
National Institutes of Health
National Institute of Mental Health
Organization Chart
[Top]
Appropriation Language
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
For carrying out section 301 and title IV of the PHS Act with respect to mental health, [$1,548,390,000]$1,459,700,000.
[Top]
Amounts Available for Obligation
| Source of Funding | FY 2015 Actual |
FY 2016 Enacted |
FY 2017 President's Budget |
|---|---|---|---|
| Mandatory Appropriation (non-add) | $1,463,036 | $1,548,390 | $1,518,673 |
| Type 1 Diabetes | (0) | (0) | (0) |
| Other Mandatory financing | (0) | (0) | (58,973) |
| Rescission | 0 | 0 | 0 |
| Sequestration | 0 | 0 | 0 |
| FY 2015 First Secretary's Transfer | 0 | 0 | 0 |
| FY 2015 Second Secretary's Transfer | 0 | 0 | 0 |
| Subtotal, adjusted appropriation | $1,463,036 | $1,548,390 | $1,518,673 |
| OAR HIV/AIDS Transfers | -29,385 | -29,717 | 0 |
| National Children's Study Transfers | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | 1,433,651 | 1,518,673 | 1,518,673 |
| Unobligated balance, start of year | 0 | 0 | 0 |
| Unobligated balance, end of year | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | $1,433,651 | $1,518,673 | $1,518.673 |
| Unobligated balance lapsing | -48 | 0 | 0 |
| Total obligations | $1,433,603 | $1,518,673 | $1,518,673 |
1 Excludes the following amounts for reimbursable activities carried out by this account: FY 2015 - $5,403 FY 2016 - $10,050 FY 2017 - $10,050
[Top]
Budget Mechanism
| MECHANISM | FY 2015 Actual |
FY 2016 Enacted |
FY 2017 President's Budget[3] |
FY 2017 +/- FY 2016 |
||||
|---|---|---|---|---|---|---|---|---|
| No. | Amount | No. | Amount | No. | Amount | No. | Amount | |
| Research Projects | ||||||||
| Noncompeting | 1,407 | $636,552 | 1,411 | $686,634 | 1,358 | $676,907 | -53 | -$9,727 |
| Administrative Supplements | (130) | 20,375 | (60) | 10,000 | (60) | 10,000 | ||
| Competing: | ||||||||
| Renewal | 74 | 38,554 | 77 | 40,360 | 84 | 39,904 | 7 | -456 |
| New | 431 | 201,727 | 452 | 211,175 | 439 | 208,789 | -13 | -2,386 |
| Supplements | 2 | 770 | 2 | 806 | 2 | 797 | 0 | -9 |
| Subtotal, Competing: | 507 | $241,051 | 531 | $252,341 | 525 | $249,490 | -6 | -$2,851 |
| Subtotal, RPGs | 1,914 | $897,978 | 1,942 | $948,975 | 1,883 | $936,397 | -59 | -$12,578 |
| SBIR/STTR | 77 | 38,974 | 83 | 43,744 | 84 | 44,404 | 1 | 660 |
| Research Project Grants | 1,991 | $936,952 | 2,025 | $992,719 | 1,967 | $980,801 | -58 | $-11,918 |
| Research Centers | ||||||||
| Specialized/Comprehensive | 39 | $69,949 | 39 | $72,839 | 39 | $72,839 | 0 | $0 |
| Clinical Research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biotechnology | 0 | 472 | 0 | 0 | 0 | 0 | 0 | 0 |
| Comparative Medicine | 0 | 990 | 0 | 0 | 0 | 0 | 0 | 0 |
| Research Centers in Minority Institutions | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Research Centers | 39 | $71,411 | 39 | $72,839 | 39 | $72,839 | 0 | $0 |
| Other Research | ||||||||
| Research Careers | 319 | $51,433 | 319 | $52,462 | 319 | $52,462 | 0 | $0 |
| Cancer Education | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cooperative Clinical Research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biomedical Research Support | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Minority Biomedical Research Support | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other | 56 | 26,954 | 56 | 27,493 | 56 | 27,493 | 0 | 0 |
| Other Research | 375 | $78,387 | 375 | $79,955 | 375 | $79,955 | 0 | $0 |
| Total Research Grants | 2,405 | $1,086,750 | 2,439 | $1,145,513 | 2,381 | $1,133,595 | -58 | $-11,918 |
| Ruth L. Kirschstein Training Awards | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 228 | $9,375 | 224 | $9,630 | 224 | $9,823 | 0 | $193 |
| Institutional Awards | 482 | 24,603 | 501 | 27,831 | 501 | 28,166 | 0 | 335 |
| Total Research Training | 710 | $33,978 | 725 | $37,461 | 725 | $37,989 | 0 | $528 |
| Research & Develop. Contracts | 156 | $75,494 | 175 | $87,558 | 175 | $94,922 | 0 | $7,364 |
| SBIR/STTR (non-add)[2] | (1) | (328) | (1) | (327) | (1) | (327) | (0) | (0) |
| Intramural Research | 268 | $164,438 | 268 | $170,892 | 268 | $172,601 | 0 | $1,709 |
| Research Management and Support | 268 | 72,991 | 273 | 77,249 | 273 | 79,566 | 0 | 2,317 |
| Research Management and Support (SBIR Admin) (non-add)[2] |
(0) | (150) | (0) | (150) | (0) | (150) | (0) | (0) |
| Office of the Director - Appropriation[2] | ||||||||
| Office of the Director - Other | ||||||||
| Buildings and Facilities | ||||||||
| Appropriation | ||||||||
| Type 1 Diabetes | ||||||||
| Program Evaluation Financing | ||||||||
| Cancer Initiative Mandatory Financing | ||||||||
| Other Mandatory Financing | -58,973 | -58,973 | ||||||
| Subtotal, Labor/HHS Budget Authority | $1,433,651 | $1,518,673 | $1,459,700 | $-58,973 | ||||
| Total, NIH Discretionary B.A. | $1,433,651 | $1,518,673 | $1,459,700 | $-58,973 | ||||
| Proposed Law Funding | ||||||||
| Other Mandatory Financing | 58,973 | 58,973 | ||||||
| Total, NIH Budget Authority | $1,433,651 | $1,518,673 | $1,518,673 | |||||
| Total, Program Level | $1,433,651 | $1,518,673 | $1,518,673 | |||||
1 All Subtotal and Total numbers may not add due to rounding.
2 All numbers in italics and brackets are non-add.
3Includes mandatory financing.
[Top]
Major Changes in the Fiscal Year 2017 President's Budget Request
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanism and activity details and these highlights will not sum to the total change for FY 2017 President’s Budget request for NIMH, which is equal to the FY 2016 Enacted level, for a total of $1,518.673 million.
Early Psychosis Intervention Network
In FY 2017, NIMH will build on previous work and launch the Early Psychosis Intervention Network (EPINET), with the goal of creating a learning health care system among early psychosis treatment clinics. With patients’ consent, EPINET clinics will create a common database with information gathered during routine clinical encounters. This database will allow clinicians and researchers to learn more about the effectiveness of early psychosis treatment. The budget request includes an additional $6.0 million for this Network.
NRSA Research Training
NIMH has provided an additional $0.528 million for NRSA Research Training to provide a stipend increase of 2.0 per cent for all trainees and maintain the same number full-time trainee positions as the FY 2016 Enacted level.
Research Project Grants
Non-competing Research Project Grants has decreased by 53 grants and $9.727 million. Competing Research Project Grants has decreased by 6 grants and $2.851 million. The funds will be used to fund other high priority areas.
Research Management and Support
This budget activity has increased by $2.317 million to pay for mandatory pay and benefit increases as well as increases needed to support the enhanced oversight and management of new and highly complex scientific programs initiated over the past five years which are critical to the success of the Institute.
Research and Development Contracts
NIMH has provided an additional $7.364 million to this budget activity to support the EPINET program as well as increased costs of purchases from other government accounts.
[Top]
Summary of Changes
| FY 2016 Enacted | $1,518,673 |
|---|---|
| FY 2017 President’s Budget | $1,518,673 |
| Net Change | $0 |
| Changes | FY 2017 President’s Budget[1] |
Change from FY 2016 | ||
|---|---|---|---|---|
| FTEs | Budget Authority | FTEs | Budget Authority | |
| A. Built-in: | ||||
| 1. Intramural research: | ||||
| a. Annualization of January 2016 pay increase & benefits | $58,188 | $266 | ||
| b. January FY 2017 pay increase & benefits | 58,188 | 749 | ||
| c. Two less days of pay | 58,188 | -423 | ||
| d. Differences attributable to change in FTE | 58,188 | 0 | ||
| e. Payment for centrally furnished services | 30,539 | 745 | ||
| f. Increased cost of laboratory supplies, materials, other expenses, and non-recurring costs | 83,874 | 373 | ||
| Subtotal | $1,709 | |||
| 2. Research management and support: | ||||
| a. Annualization of January 2016 pay increase & benefits | $37,425 | $175 | ||
| b. January FY 2017 pay increase & benefits | 37,425 | 486 | ||
| c. Two less days of pay | 37,425 | -276 | ||
| d. Differences attributable to change in FTE | 37,425 | 0 | ||
| e. Payment for centrally furnished services | 9,187 | 465 | ||
| f. Increased cost of laboratory supplies, materials, other expenses, and non-recurring costs | 32,953 | 1,467 | ||
| Subtotal | $2,317 | |||
| Subtotal, Built-in | $4,026 | |||
1 Includes mandatory financing.
| Changes | FY 2017 President’s Budget[1] |
Change from FY 2016 | ||
|---|---|---|---|---|
| No. | Amount | No. | Amount | |
| B. Program: | ||||
| 1. Research Project Grants: | ||||
| a. Noncompeting | 1,358 | $686,907 | -53 | -$9,727 |
| b. Competing | 525 | 249,490 | -6 | -2,851 |
| c. SBIR/STTR | 84 | 44,404 | -1 | 660 |
| Subtotal, RPGs | 1,967 | $980,801 | -58 | -$11,918 |
| 2. Research Centers | 39 | $72,839 | 0 | $0 |
| 3. Other Research | 375 | 79,955 | 0 | 0 |
| 4. Research Training | 725 | 37,989 | 0 | 528 |
| 5. Research and Development Contracts | 175 | 94,922 | 0 | 7,364 |
| Subtotal, Extramural | $1,266,506 | -$4,026 | ||
| FTEs | FTEs | |||
| 6. Intramural research | 268 | $172,601 | 0 | $0 |
| 7. Research Management and Support | 273 | 79,566 | 0 | 0 |
| 8. Construction | 0 | 0 | ||
| 9. Buildings and Facilities | 0 | 0 | ||
| Subtotal, program | 541 | $1,518,673 | 0 | -$4,026 |
| Total changes | $0 | |||
[Top]
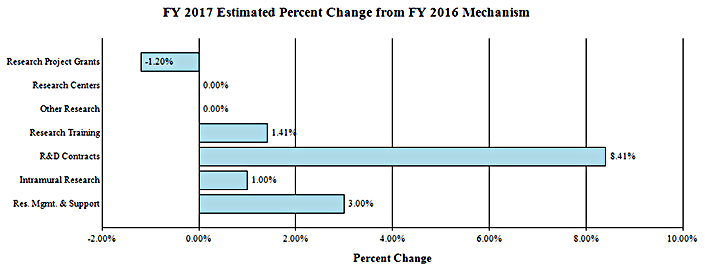
Budget Graphs
History of Budget Authority and FTEs:
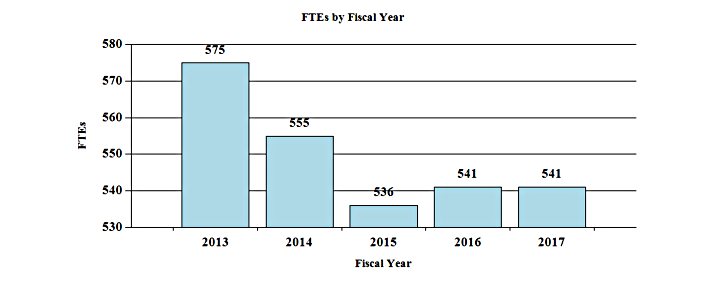
Distribution by Mechanism:
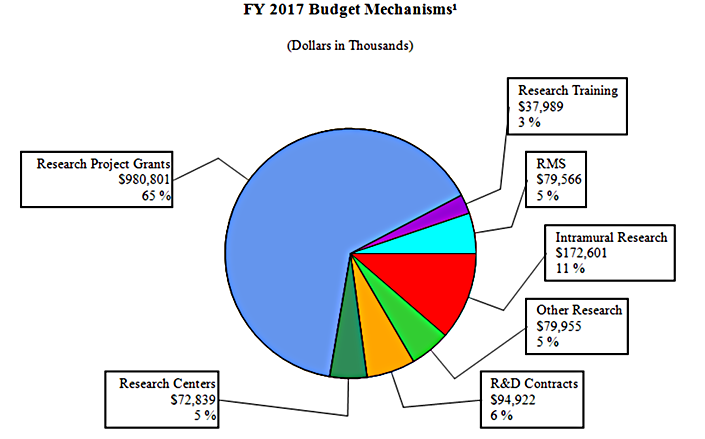
Change by Selected Mechanism:
Budget Authority by Activity
| FY 2015 Actual |
FY 2016 Enacted |
FY 2017 President's Budget[2] |
FY 2017 +/- FY 2016 |
|||||
|---|---|---|---|---|---|---|---|---|
| FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount | |
| Extramural Research, Detail: | ||||||||
| Neuroscience & Basic Behavioral Science | $523,098 | $554,171 | $552,181 | -$1,990 | ||||
| Services & Intervention Research | 138,048 | 147,097 | 146,568 | -529 | ||||
| Translational Research | 366,856 | 391,055 | 389,650 | -1,405 | ||||
| AIDS Research | 145,602 | 149,769 | 149,769 | 0 | ||||
| Office of the Director | 22,618 | 28,440 | 28,338 | -102 | ||||
| Subtotal, Extramural | $1,196,222 | $1,270,532 | $1,266,506 | -$4,026 | ||||
| Intramural research | 268 | $164,438 | 268 | $170,892 | 268 | $172,601 | 0 | $1,709 |
| Research Management & Support | 268 | $72,991 | 273 | $77,249 | 273 | $79,566 | 0 | $2,317 |
| TOTAL | 536 | $1,433,651 | 541 | $1,518,673 | 541 | $1,518,673 | 0 | $0 |
2 Includes mandatory financing.
[Top]
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2016 Amount Authorized | FY 2016 Enacted | 2017 Amount Authorized | FY 2017 President's Budget[1] |
|
|---|---|---|---|---|---|---|
| Research and Investigation | Section 301 | 42§241 | Indefinite | $1,518,673,000 | Indefinite | $1,459,700,000 |
| National Institute of Mental Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||
| Total, Budget Authority | $1,518,673,000 | $1,459,700,000 |
[Top]
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation |
|---|---|---|---|---|
| 2007 | $1,394,806,000 | $1,394,806,000 | $1,403,551,000 | $1,404,494,000 |
| Rescission | $0 | |||
| 2008 | $1,405,421,000 | $1,425,531,000 | $1,436,001,000 | $1,429,466,000 |
| Rescission | $24,973,000 | |||
| Supplemental | $7,475,000 | |||
| 2009 | $1,406,841,000 | $1,455,145,000 | $1,445,987,000 | $1,450,491,000 |
| Rescission | $0 | |||
| 2010 | $1,474,676,000 | $1,502,266,000 | $1,475,190,000 | $1,489,372,000 |
| Rescission | $0 | |||
| 2011 | $1,540,345,000 | $1,537,942,000 | $1,489,372,000 | |
| Rescission | $13,078,800 | |||
| 2012 | $1,517,006,000 | $1,517,006,000 | $1,460,671,000 | $1,483,068,000 |
| Rescission | $2,802,999 | |||
| 2013 | $1,479,204,000 | $1,483,687,000 | $1,480,265,001 | |
| Rescission | $2,960,530 | |||
| Sequestration | ($74,299,124) | |||
| 2014 | $1,465,782,000 | $1,456,041,000 | $1,446,172,000 | |
| Rescission | $0 | |||
| 2015 | $1,440,076,000 | 1,463,036,000 | ||
| Rescission | $0 | |||
| 2016 | $1,489,417,000 | $1,512,401,000 | $1,520,260,000 | $1,548,390,000 |
| 2017[1] | $1,518,673,000 |
[Top]
Justification of Budget Request
Authorizing Legislation:
Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2015 Actual |
FY 2016 Enacted |
FY 2017 President's Budget |
FY 2017 +/- FY 2016 | |
|---|---|---|---|---|
| BA | $1,433,651,000 | $1,518,673,000 | $1,518,673,000 | +$0 |
| FTE | 536 | 541 | 541 | 0 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements;
Contracts; Direct Federal/Intramural and Other.
Director’s Overview
The National Institute of Mental Health (NIMH) is the lead Federal agency for research on mental illnesses, with a mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure.
In the United States, an estimated 43.6 million adults suffer from a mental illness.1 Mental illnesses are significantly impairing and can be life-threatening; they were the leading cause of disability in the United States in 2010, accounting for 18.7 percent of all years of life lost to illness, disability, or premature death.2 Suicide is the second leading cause of death in youth and young adults aged 15-34, accounting for the loss of more than 41,000 American lives each year, and is the tenth leading cause of death overall in the United States.3 A cautious estimate places the direct and indirect financial costs associated with mental illness in the United States at well over $300 billion annually, and mental illnesses rank as the third most costly medical conditions in terms of overall health care expenditures, behind only heart conditions and traumatic injury.4,5
To ensure that NIMH optimizes its priorities and invests wisely in the most rigorous science, the Institute released an updated Strategic Plan for Research in March 2015.6 The plan provides a framework to accelerate the pace of scientific progress by generating research that will have the greatest public health impact and continue to fuel the transformation of mental health care. The four Objectives of the Plan describe the continuum of mental health research: defining the mechanisms of complex behavior; charting mental illness trajectories to determine when, where, and how to intervene; striving for prevention and cures; and, strengthening the public health impact of NIMH-supported research. These Objectives form a roadmap for NIMH’s priorities over the next five years. In addition, NIMH has taken steps to improve efficiency, increase transparency, and monitor human-subjects protection and privacy issues effectively in its clinical research portfolio.7 NIMH will continue to monitor carefully the initiation, recruitment, and completion of each clinical trial, with continued funding contingent upon meeting milestones.
1 SAMHSA, Results from the 2014 National Survey on Drug Use and Health: Mental Health Findings, NSDUH Series H-47, HHS Publication No. (SMA) 13-4805. Rockville, MD: SAMHSA, 2014.
2 US Burden of Disease Collaborators. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA, 310(6): 591-608, 2013.
3 CDC, NCIPC. WISQARS: www.cdc.gov/ncipc/wisqars accessed October 2015.
4 Insel TR. Assessing the economic cost of serious mental illness. Am J Psychiatry. 2008 Jun;165(6):663-5.
5 Soni A. The Five Most Costly Conditions, 1996 and 2006: Estimates for the U.S. Civilian Noninstitutionalized Population. Statistical Brief #248. July 2009. AHRQ, Rockville, MD.
6 http://www.nimh.nih.gov/about/strategic-planning-reports/index.shtml
Basic Research, the Foundation for Success
The Brain Research through Advancing Innovative Neurotechnologies BRAIN Initiative is supporting the creation of new tools for decoding the language of the brain8. Managed by 10 NIH Institutes and Centers (ICs) and co-led by NIMH and the National Institute of Neurological Disorders and Stroke, the BRAIN Initiative made great strides towards uncovering the causal mechanisms of brain circuit function in FY 2015. NIMH-funded researchers published findings on a new technique for single-cell analysis, called Drop-Seq, that is faster and less expensive than current, more labor-intensive methods, and yet just as accurate. Other researchers have developed technology for targeting and precisely affecting a specific brain cell type (Designer Receptor Exclusively Activated by Designer Drugs, or DREADDs). NIMH continues to prioritize research aimed at developing innovative tools and technologies dedicated to mapping aberrant brain activity associated with mental illnesses.
NIMH investments in basic neuroscience research have built a foundation for future BRAIN Initiative efforts. For example, NIMH-funded researchers took a technology, called induced pluripotent stem cells (in which they turned stem cells derived from patients’ skin cells into neurons), and streamlined the procedure to generate cortex-like structures of neurons and their support cells, called spheroids, that mimic the developing brain. These spheroids function so similarly to the developing brain that they will eventually enable researchers to evaluate proposed brain mechanisms underlying mental illnesses – the ‘disease-in-a-dish’ approach – and in turn, design more accurate treatments. This work illustrates how basic research provides the platform for successful treatment development.
Improving Precision through Information Integration
Increased precision in mental health research requires a framework for integrating many levels of information to understand basic dimensions of functioning underlying the full range of human behavior. The NIMH Research Domain Criteria (RDoC) initiative expands precision medicine to all areas of mental health research.9 RDoC enables clinical investigators to think outside the box of current diagnostic categories, and encourages basic scientists to identify mechanisms of specific domains of mental function. For example, the Bipolar Schizophrenia Network on Intermediate Phenotypes (BSNIP) study used the RDoC approach to examine individuals across multiple diagnostic groups in the psychosis spectrum, employing statistical techniques to look for patterns in the data. This approach resulted in natural groupings of patients based on their biological information, rather than only observable symptoms.10
Another ongoing NIMH-funded study is using the RDoC approach as it applies to the genetic basis of attention deficit hyperactivity disorder (ADHD). Specifically, investigators are working with existing genetic databases to differentiate gene pathways to ADHD, and are then using these pathways to develop subgroups that can be validated with neurocognitive measures and structural connectivity analyses. Determining the biological basis of ADHD subgroups can lead the way towards future diagnostic and treatment development efforts, exemplifying the RDoC approach of integrating basic genetic findings into actionable translational science.
8 http://www.nih.gov/science/brain/index.htm
9 http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml
10 See: http://www.ncbi.nlm.nih.gov/pubmed/26462502
Big Data and Technology
NIMH is committed to supporting data integration across studies and the broad sharing of data and the resources necessary to accelerate scientific progress. Moreover, data sharing is an expectation for all NIMH-funded clinical research. NIMH has federated a series of repositories for this purpose – referred to in aggregate as the NIMH Data Archive: the NationalDatabase for Autism Research, the NIH Pediatric MRI Data Repository, the RDoC Database, and the National Database for Clinical Trials Related to Mental Illness. The NIMH commitment to broad sharing of data is also evident in its ongoing support of the Psychiatric Genomics Consortium (PGC), the largest ever genomic investigation of brain disorders, involving hundreds of thousands of samples from more than 80 institutions in over 30 countries.11,12,13,14,15 Recently, PGC researchers identified overlapping genetic risk among schizophrenia, bipolar disorder, and depression for pathways affecting the immune system and brain cell communication. These findings will help guide the development of treatments for mental illnesses, thereby enabling NIMH to continue onward in accomplishing its mission.
Budget Policy: The FY 2017 President’s Budget estimate is $1,518.673 million, the same as the FY 2016 Enacted level.
12 http://www.pediatricmri.nih.gov/
13 http://rdocdb.nimh.nih.gov/
Program Descriptions
Neuroscience and Basic Behavioral Science
The Division of Neuroscience and Basic Behavioral Science provides support for research in the areas of basic neuroscience, genetics, basic behavioral science, research training, resource development, and drug discovery. In cooperation with other NIMH programs and the wider research community, this program ensures that relevant basic scientific knowledge is generated and used in pursuit of improved methods to diagnose, treat, and prevent mental illnesses.
NIMH funds grants across a range of research topics to enhance our comprehension of the basic neurobiology underlying mental illnesses. In FY 2017, NIMH will continue to capitalize on data arising from large scale genomic studies to understand the genetic underpinnings of mental illnesses. In particular, studies of autism spectrum disorder (ASD) and schizophrenia have yielded a large number of regions of the genome associated with disease. NIMH will work to fine tune these associations, using new statistical methods as well as biological studies.
Budget Policy: The FY 2017 President’s Budget estimate is $552.181 million, a decrease of $1.990 million or 0.4 percent compared to the FY 2016 Enacted level.
Program Portrait: Mapping the Brain’s Connections across the Lifespan
| FY 2016 Level: | $21.3 million |
|---|---|
| FY 2017 Level: | $24.6 million |
| Difference: | +$3.3 million |
Over the past decade, an explosion of interest in the patterns of connectivity underlying structural and functional brain networks has resulted in a shift to studying connectivity and networks, revolutionizing how we understand brain function and dysfunction. Echoing this shift, the NIH Human Connectome Project (HCP), funded since 2010 by the NIH Blueprint for Neuroscience Research, is a large-scale effort to develop a comprehensive reference atlas of neuronal connectivity – that is, a connectome.16 HCP is mapping brain connectivity in 1,200 healthy adults, and making this data freely available to the scientific community. This project aims to increase knowledge of what makes us uniquely human, and also sets the stage for studies of abnormal brain circuits that appear in many mental illnesses.
Early findings from HCP show promise for improving our understanding of how brain connectivity is related to human behavior. A study published in September 2015 used HCP data to determine whether any specific patterns of brain connectivity are associated with specific sets of correlated demographics and behavior.17 The investigators discovered that the strongest correlation emerged between an individual’s connectome and “positive” measures, such as higher vocabulary, better memory, and higher life satisfaction. NIH has also funded a Connectome Coordination Facility that will maintain the existing data repository, support a help desk to facilitate community use of the resource, and serve as a harmonization center where data from multiple labs are made compatible.
In FY 2015, NIMH extended its connectome efforts by releasing a new series of funding opportunity announcements to support the study of infants and youth, in order to capture the structural and functional changes that occur in the brain during typical development, as well as in clinical populations.18,19,20 The National Institute on Aging is coordinating a similar expansion to study older adults.21 These expansions across the lifespan will enhance the clinical relevance of the data and provide benchmarks for understanding the causes of human brain disorders. Review of applications is currently ongoing, with funding of meritorious proposals anticipated to begin in the summer of 2016. NIMH supports about 30 percent of this NIH Blueprint for Neuroscience Research project.
16 http://www.neuroscienceblueprint.nih.gov/connectome/
17 http://www.ncbi.nlm.nih.gov/pubmed/26414616
18 http://grants.nih.gov/grants/guide/rfa-files/RFA-MH-16-160.html
19 http://grants.nih.gov/grants/guide/rfa-files/RFA-MH-16-150.html
20 http://grants.nih.gov/grants/guide/pa-files/PAR-14-281.html
21 http://grants.nih.gov/grants/guide/rfa-files/RFA-AG-16-004.html
Translational Research
The Division of Translational Research (DTR) supports integrative, multidisciplinary research and training programs that translate findings from basic science in order to discover the causes, mechanisms, and trajectories of mental illnesses, and to develop effective interventions for children and adults. DTR supports research on the characteristics of and risk factors for psychiatric disorders; the neurobehavioral mechanisms of psychopathology; the trajectories of risk and resilience based on the interactive influences of genetics, brain development, environment, and experience; and the design and testing of innovative treatments and interventions.
In FY 2015, DTR launched the Autism Biomarkers Consortium project. The Autism Biomarkers Consortium is supported by the Biomarkers Consortium, a large public-private partnership that aims to facilitate precision medicine by supporting research to identify disease-specific biomarkers for targeted and individualized treatment. The project will receive a total of $28 million from the Biomarkers Consortium over the next four years to test and refine clinical measures of social impairment in ASD, in order to evaluate potential behavioral and drug therapies as rigorously as possible. Autism Biomarkers Consortium researchers will collect electroencephalogram and eye-tracking measures in 325 children with ASD to identify reliable biomarkers for the objective selection of biologically similar subgroups of children with ASD for optimized treatment. In 2016 and beyond, the study will begin generating a scientific community resource by making the biomarker measures, laboratory tests of social impairment, extensive phenotypic information, and blood samples from the children and their parents available for use in future studies.
In FY 2016, DTR plans to launch a five-year, multi-site initiative, “Longitudinal Assessment of Post-traumatic Syndromes (LAPS),” to develop a new understanding of the neurobiological mechanisms responsible for mental illness following trauma, pending the receipt of meritorious grant applications. This effort will facilitate more accurate diagnosis, and more effective prevention and treatment of the spectrum of trauma symptoms traditionally characterized as post-traumatic stress disorder (PTSD). LAPS will assess patients exposed to trauma to characterize post-traumatic changes in neurobiological factors, cognitive functioning, and other markers of risk over time; develop algorithms to predict different clinical trajectories following trauma exposure; and inform interventions that target the underlying causes of symptoms in subgroups of patients that are less heterogeneous than individuals with a traditional PTSD diagnosis. LAPS has the potential to improve care for individuals at high risk for post-traumatic stress conditions dramatically, across civilian, military, and veteran populations. LAPS is also responsive to White House calls to invest in research that will establish biomarkers, define the pathophysiology, and develop new treatments based on mechanisms for post-traumatic stress spectrum illnesses.22
Budget Policy: The FY 2017 President’s Budget estimate is $389.650 million, a decrease of $1.405 million or 0.4 percent compared to the FY 2016 Enacted level.
Services and Intervention Research
The Division of Services and Intervention Research (DSIR) supports research that evaluates the effectiveness of psychosocial, pharmacological, somatic, rehabilitative, and combined interventions to prevent or treat mental and behavioral illnesses. DSIR evaluates interventions for children, adolescents, and adults, focusing on acute and long-term symptom reduction, remission, and improved community functioning. DSIR also supports mental health services research, including interventions to improve the quality and outcomes of care; organization and system-level interventions to enhance service delivery; and, strategies for widespread dissemination and implementation of evidence-based treatments into routine care settings.
In FY 2015, DSIR supported two large-scale initiatives to improve the effectiveness of mental health services delivered at critical periods of illness or across developmental life stages. One initiative concerns suicide prevention. Suicide risk is 10 times higher among persons recently released from jail or prison, compared to individuals from the general population.23 To reduce suicide risk during this critical period, NIMH, in partnership with the NIH Office of Behavioral and Social Sciences Research and the National Institute of Justice, funded the Suicide Prevention for at-Risk Individuals in Transition (SPIRIT) study.24 This randomized control trial will evaluate the effectiveness of an evidence-based Safety Planning Intervention for reducing suicide events in the year following incarceration. The second initiative concerns outcomes for people with ASD. ASD begins in early childhood, but impairments often endure through transitions to adolescence and adulthood. There are few studies to guide delivery of mental health services across these life stages. ASD services research initiative is supporting 12 studies that examine strategies for improving outcomes for people with ASD across the lifespan. Of note, five of the 12 studies are focused on early childhood. The investigators of these studies have formed the ASD Pediatric Early Detection and Engagement in Service (ASD PEDS) network, which will pool data across the projects to expand capacity significantly to address key services research questions for young children aged 0-2 years, a developmentally important time in the course of ASD.
Budget Policy: The FY 2017 President’s Budget estimate is $146.568 million, a decrease of $0.529 million or 0.4 percent compared to the FY 2016 Enacted level.
23 See http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4579558/
24 See http://www.nimh.nih.gov/news/science-news/2015/embracing-the-spirit-of-reducing-suicide.shtml
Program Portrait: Addressing Psychosis through a Learning Health Care System Approach
| FY 2016 Level: | $9.5 million |
|---|---|
| FY 2017 Level: | $15.5 million |
| Difference: | +$6.0 million |
The ‘learning health care system’ approach allows clinicians and researchers to learn about the effectiveness of treatments in use and to develop new strategies based on a constant flow of data from patients in real-world settings. The realm of diagnosing and treating psychosis is primed to benefit from this approach. Many people experiencing a first episode of psychosis (FEP) experience significant delays in seeking and obtaining care, though treatment is most effective for people who receive care soon after psychotic symptoms begin. The Recovery After an Initial Schizophrenia Episode (RAISE) initiative, which NIMH launched in 2008, aims to change the downward spiral that can result from untreated psychosis, and help return people to a path toward productive, independent lives. RAISE is a large-scale research initiative that began with two studies examining different aspects of coordinated specialty care (CSC) treatments for people who were experiencing FEP.
CSC is a recovery-oriented treatment program for people with FEP. CSC uses a team of specialists who work with the client to create a personal treatment plan. The specialists offer psychotherapy, medication management, family education, case management, and work or education support, depending on the individual’s needs and preferences. The goal is to link the client with a CSC team as soon as possible after psychotic symptoms begin. The client and the CSC team work together to make treatment decisions, involving family members as much as possible. RAISE investigators have shown that CSC is effective and can be implemented in community treatment settings nationwide.
Moving forward, increased funding will enable NIMH to build on the work accomplished thus far in the RAISE initiative by launching the Early Psychosis Intervention Network (EPINET), with the goal of creating a learning health care system among early psychosis treatment clinics. With patients’ consent, EPINET clinics will create a common database with information gathered during routine clinical encounters. This database will allow clinicians and researchers to learn more about the effectiveness of early psychosis treatment. EPINET will also accelerate studies of psychosis risk factors, biomarkers of illness, and pre-emptive interventions through enhancements related to, for example, data capture, data processing, and the development of specialty toolkits. RAISE and EPINET exemplify NIMH’s determination to ensure that lessons learned from research and clinical experiences are systematically and rapidly put to use to improve the lives of individuals with psychosis and their families.
AIDS Research
The Division of AIDS Research (DAR) supports research and research training spanning the priority areas outlined in the NIH HIV/AIDS Research Priorities and Guidelines for Determining AIDS Funding.25 DAR supports behavioral and social science research critical to the goal of reducing HIV/AIDS incidence through developing and testing new prevention strategies, such as vaccines, microbicides, and pre-exposure prophylaxis approaches. Behavioral and social science research is critical to understanding individual and communal acceptance of prevention strategies, so that the delivery of such strategies is fully optimized, widely disseminated, and successfully implemented. Moreover, DAR research places especial emphasis on health disparities, and in particular, on mental illnesses that may increase risk for HIV infection or have a negative impact on health outcomes.
25 See https://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-137.html
DAR is also actively participating in cure efforts with the support of research on methods to eliminate HIV in infected individuals by eradicating or silencing the virus from biological reservoirs in the central nervous system (CNS). As many drugs designed to eradicate the virus are unable to penetrate the protected environment of the CNS, the CNS can act as an unwitting reservoir for HIV. Therefore, HIV latency is critically important to consider in studies of eradication and reactivation, and DAR supports research on viral latency and persistence in the CNS. This work may also inform methods to prevent or treat the neurological comorbidities of HIV, with a particular emphasis on the premature aging associated with long-term HIV disease and antiretroviral therapy. Through its commitment to bringing multidisciplinary expertise to agency-wide strategic planning efforts, DAR is working to ensure that effective integration of biomedical and behavioral approaches is accomplished, bringing us ever closer to an AIDS-free generation.
Budget Policy: The FY 2017 President’s Budget estimate is $149.769 million, the same as the FY 2016 Enacted level.
Intramural Research Programs
The Division of Intramural Research Programs (IRP) is the internal research component of NIMH, complementing the Institute’s extramural grant funding program. IRP scientists investigate basic, translational, and clinical aspects of brain function and behavior, conducting state-of-the-art research through the use of unique NIH resources. In addition, DIRP provides an excellent environment for training the next generation of clinical and basic scientists.
IRP researchers continue to examine the relationship between genes, the brain, and behavior both in healthy development and in adult and childhood-onset mental illnesses. In FY 2015, many important basic science advances came out of the Division, including insight into the molecular mechanisms of how amphetamine stimulates brain cells; linking specific patterns of brain activity, called ‘neuronal avalanches,’ to changes in physiological state; and demonstrating how the immune system interacts with the brain to affect mood. IRP scientists use brain imaging to study disruptive behavior disorders in youth, which confer increased risk of substance abuse and criminal behavior, and they investigate innovative behavioral treatments for children with severe mood dysregulation or anxiety. IRP researchers are also exploring novel medications for treatment-resistant depression in adults, including ketamine and other experimental fast-acting antidepressant medications, and working to identify biomarkers for predicting how well an individual with depression will respond to such rapid-acting antidepressants. In FY 2015, IRP recruited three new tenure-track scientists who will study how stress affects memory and behavior, investigate brain mechanisms that underlie cognitive behavior, and use neuroimaging and genomic approaches to examine human brain development.
Budget Policy: The FY 2017 President’s Budget estimate is $172.601 million, an increase of $1.709 million or 1.0 percent compared to the FY 2016 Enacted level.
Research Management and Support (RMS)
RMS provides leadership to NIMH, as well as administrative, budgetary, logistical, and scientific support in the review, award, and monitoring of research grants, training grants, and research and development contracts. RMS functions include strategic planning, coordination, and evaluation of NIMH’s programs; regulatory compliance; coordinating global mental health efforts; and, liaising with other Federal agencies, Congress, and the public. In FY 2015, NIMH managed 2,405 research grants, 324 training grants that supported 710 full-time trainee positions, and 156 research and development contracts.
Budget Policy: The FY 2017 President’s Budget estimate is $79.566 million, an increase of $2.317 million or 3.0 percent compared to the FY 2016 Enacted level. The funds are needed because of additional personnel and operating expenses related to the scale up of the EPINET and HCP Initiatives.
Budget Authority by Object Class [1]
| FY 2016 Enacted |
FY 2017 President's Budget[2] |
FY 2017 +/- FY 2016 | |
|---|---|---|---|
| Total compensable workyears: | |||
| Full-time employment | 541 | 541 | 0 |
| Full-time equivalent of overtime and holiday hours | 0 | 0 | 0 |
| Average ES salary | $155 | $158 | $2 |
| Average GM/GS grade | 12.7 | 12.7 | 0.0 |
| Average GM/GS salary | $106 | $108 | $2 |
| Average salary, grade established by act of July 1, 1944 (42 U.S.C. 207) | $135 | $136 | $1 |
| Average salary of ungraded positions | $133 | $137 | $4 |
| OBJECT CLASSES | FY 2016 Enacted | FY 2017 President's Budget[2] | FY 2017 +/- FY 2016 |
| Personnel Compensation: | |||
| 11.1 Full-time Permanent | $40,049 | $40,356 | $307 |
| 11.3 Other Than Full-Time Permanent | 23,020 | 23,196 | 176 |
| 11.5 Other Personnel Compensation | 1,413 | 1,423 | 11 |
| 11.7 Military Personnel | 270 | 272 | 2 |
| 11.8 Special Personnel Services Payments | 9,035 | 9,104 | 69 |
| 11.9 Subtotal, Personnel Compensation | $73,787 | $74,352 | $565 |
| 12.1 Civilian Personnel Benefits | $20,744 | $21,155 | $411 |
| 12.2 Military Personnel Benefits | 106 | 106 | 1 |
| 13.0 Benefits for Former Personnel | 0 | 0 | 0 |
| Subtotal, Pay Costs | $94,636 | $95,613 | $977 |
| 21.0 Travel and Transportation of Persons | $2,622 | $2,668 | $46 |
| 22.0 Transportation of Things | 93 | 95 | 2 |
| 23.1 Rental Payments to GSA | 1 | 1 | 0 |
| 23.2 Rental Payments to Others | 0 | 0 | 0 |
| 23.3 Communications, Utilities and Misc. Charges | 1,182 | 1,206 | 23 |
| 24.0 Printing and Reproduction | 51 | 52 | 2 |
| 25.1 Consulting Services | $1,678 | $1,751 | $73 |
| 25.2 Other Services | 29,663 | 30,019 | 356 |
| 25.3 Purchase of Goods and Services from Government Accounts | 152,735 | 159,594 | 6,859 |
| 25.4 Operation and Maintenance of Facilities | $4,484 | $4,485 | $0 |
| 25.5 Research and Development Contracts | 34,446 | 37,326 | 2,880 |
| 25.6 Medical Care | 275 | 276 | 2 |
| 25.7 Operation and Maintenance of Equipment | 2,918 | 2,941 | 22 |
| 25.8 Subsistence and Support of Persons | 0 | 0 | 0 |
| 25.0 Subtotal, Other Contractual Services | $226,200 | $236,391 | $10,191 |
| 26.0 Supplies and Materials | $4,240 | $4,294 | $54 |
| 31.0 Equipment | 6,673 | 6,769 | 95 |
| 32.0 Land and Structures | 0 | 0 | 0 |
| 33.0 Investments and Loans | 0 | 0 | 0 |
| 41.0 Grants, Subsidies and Contributions | 1,182,974 | 1,171,584 | -11,390 |
| 42.0 Insurance Claims and Indemnities | 0 | 0 | 0 |
| 43.0 Interest and Dividends | 0 | 0 | 0 |
| 44.0 Refunds | 0 | 0 | 0 |
| Subtotal, Non-Pay Costs | $1,424,037 | $1,423,060 | -$977 |
| Total Budget Authority by Object Class | $1,518,673 | $1,518,673 | $0 |
2 Includes mandatory financing.
[Top]
Salaries and Expenses
| Object Classes | FY 2016 Enacted | FY 2017 President's Budget | FY 2017 +/- FY 2016 |
|---|---|---|---|
| Personnel Compensation: | |||
| Full-time permanent (11.1) | $40,049 | $40,356 | $307 |
| Other than full-time permanent (11.3) | 23,020 | 23,196 | 176 |
| Other personnel compensation (11.5) | 1,413 | 1,423 | 11 |
| Military personnel (11.7) | 270 | 272 | 2 |
| Special personnel services payments (11.8) | 9,035 | 9,104 | 69 |
| Total Personnel Compensation (11.9) | $73,787 | $74,352 | $565 |
| Civilian personnel benefits (12.1) | $20,744 | $21,155 | $411 |
| Military personnel benefits (12.2) | 106 | 106 | 1 |
| Benefits to former personnel (13.0) | 0 | 0 | 0 |
| Subtotal, Pay Costs | $94,636 | $95,613 | $977 |
| Travel and Transportation of Persons (21.0) | $2,622 | $2,668 | $46 |
| Transportation of things (22.0) | 93 | 95 | 2 |
| Rental payments to others (23.2) | 0 | 0 | 0 |
| Communications, utilities and miscellaneous charges (23.3) | 1,182 | 1,206 | 23 |
| Printing and reproduction (24.0) | 51 | 52 | 2 |
| Other Contractual Services: | |||
| Consultant services (25.1) | 1,609 | 1,676 | 67 |
| Other services (25.2) | 29,663 | 30,019 | 356 |
| Purchases from government accounts (25.3) | 89,164 | 92,194 | 3,031 |
| Operation and maintenance of facilities (25.4) | 4,484 | 4,485 | 0 |
| Operation and maintenance of equipment (25.7) | 2,918 | 2,941 | 22 |
| Subsistence and support of persons (25.8) | 0 | 0 | 0 |
| Subtotal Other Contractual Services | $127,838 | $131,314 | $3,476 |
| Supplies and materials (26.0) | $4,240 | $4,294 | $54 |
| Subtotal, Non-Pay Costs | $136,027 | $139,629 | $3,603 |
| Total, Administrative Costs | $230,662 | $235,242 | $4,580 |
[Top]
Detail of Full-Time Equivalent Employment (FTE)
| Office/Division | FY 2015 Actual |
FY 2016 Est. |
FY 2017 Est. |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of AIDS Research | |||||||||
| Direct: | 12 | - | 12 | 13 | - | 13 | 13 | - | 13 |
| Reimbursable: | - | - | - | - | - | - | - | - | |
| Total: | 12 | - | 12 | 13 | - | 13 | 13 | - | 13 |
| Division of Extramural Activities | |||||||||
| Direct: | 46 | - | 46 | 47 | - | 47 | 47 | - | 47 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 46 | - | 46 | 47 | - | 47 | 47 | - | 47 |
| Division of Intramural Research Programs | |||||||||
| Direct: | 267 | 1 | 268 | 267 | 1 | 268 | 267 | 1 | 268 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 267 | 1 | 268 | 267 | 1 | 268 | 267 | 1 | 268 |
| Division of Neuroscience and Basic Behavioral Science | |||||||||
| Direct: | 26 | - | 26 | 27 | - | 27 | 27 | - | 27 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 26 | - | 26 | 27 | - | 27 | 27 | - | 27 |
| Division of Services and Intervention Branch | |||||||||
| Direct: | 16 | 1 | 17 | 16 | 1 | 17 | 16 | 1 | 17 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 16 | 1 | 17 | 16 | 1 | 17 | 16 | 1 | 17 |
| Division of Translational Research | |||||||||
| Direct: | 29 | - | 29 | 31 | - | 31 | 31 | - | 31 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 34 | - | 34 | 31 | - | 31 | 31 | - | 31 |
| Office of the Director | |||||||||
| Direct: | 138 | - | 138 | 138 | - | 138 | 138 | - | 138 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 138 | - | 138 | 138 | - | 138 | 138 | - | 138 |
| Total | 534 | 2 | 536 | 539 | 2 | 541 | 539 | 2 | 541 |
Includes FTEs whose payroll obligations are supported by NIH Common Fund.
| Office/Division | FY 2015 Actual |
FY 2016 Est. |
FY 2017 Est. |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| FTEs supported by funds from Cooperative Research and Development Agreements. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fiscal Year | Average GM/GS Grade |
|---|---|
| 2013 | 12.3 |
| 2014 | 12.3 |
| 2015 | 12.7 |
| 2016 | 12.7 |
| 2017 | 12.7 |
[Top]
Detail of Positions [1]
| Grade | FY 2015 Actual |
FY 2016 Enacted |
FY 2017 President's Budget |
|---|---|---|---|
| Total, ES Positions | 1 | 1 | 1 |
| Total, ES Salary | 152,758 | 155,215 | 156,397 |
| GM/GS-15 | 51 | 51 | 15 |
| GM/GS-14 | 69 | 69 | 69 |
| GM/GS-13 | 93 | 95 | 95 |
| GS-12 | 64 | 66 | 66 |
| GS-11 | 50 | 51 | 51 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 29 | 29 | 29 |
| GS-8 | 11 | 11 | 11 |
| GS-7 | 13 | 13 | 13 |
| GS-6 | 1 | 1 | 1 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 0 | 0 | 0 |
| GS-3 | 2 | 2 | 2 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 383 | 388 | 388 |
| Grades established by Act of July 1, 1944 (42 U.S.C. 207): | 0 | 0 | 0 |
| Assistant Surgeon General | 2 | 2 | 2 |
| Director Grade | 0 | 0 | 0 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 2 | 2 | 2 |
| Ungraded | 168 | 168 | 168 |
| Total permanent positions | 386 | 391 | 391 |
| Total positions, end of year | 554 | 559 | 559 |
| Total full-time equivalent (FTE) employment, end of year | 536 | 541 | 541 |
| Average ES salary | 152,758 | 155,215 | 156,397 |
| Average GM/GS grade | 12.7 | 12.7 | 12.7 |
| Average GM/GS salary | 104,512 | 106,193 | 107,901 |
