Archived Content
The National Institute of Mental Health archives materials that are over 4 years old and no longer being updated. The content on this page is provided for historical reference purposes only and may not reflect current knowledge or information.
Schizophrenia’s Genetic “Skyline” Rising
Suspect Common Variants Soar from 30 to 108 – NIH-funded Study
• Press Release
The largest genomic dragnet of any psychiatric disorder to date has unmasked 108 chromosomal sites harboring inherited variations in the genetic code linked to schizophrenia, 83 of which had not been previously reported. By contrast, the “skyline” of such suspect variants associated with the disorder contained only 5 significant peaks in 2011. By combining data from all available schizophrenia genetic samples, researchers supported by the National Institutes of Health powered the search for clues to the molecular basis of the disorder to a new level.
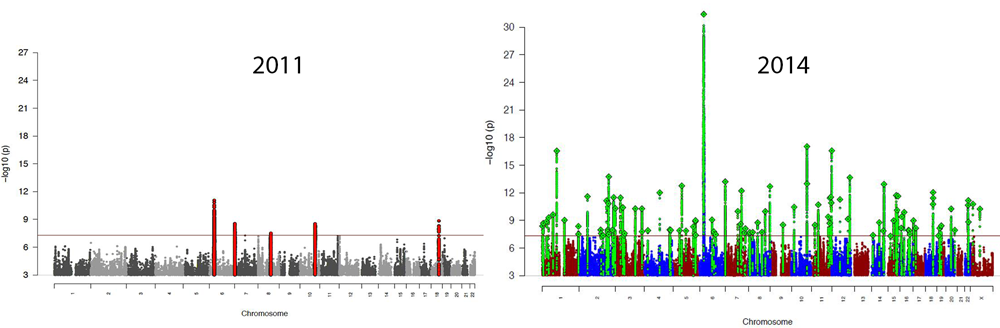
The “skyline” – Manhattan plot graph of genetic variation associated with schizophrenia – has risen dramatically over the past few years, thanks to the enhanced ability to detect subtle effects of common gene variants that comes with larger sample sizes. Bars that rise above the red line indicate chromosomal sites that confer risk.
“While the suspect variation identified so far only explains about 3.5 percent of the risk for schizophrenia, these results warrant exploring whether using such data to calculate an individual’s risk for developing the disorder might someday be useful in screening for preventive interventions,” explained Thomas R. Insel, M.D., director of the NIH’s National Institute of Mental Health, a funder of the study. “Even based on these early predictors, people who score in the top 10% of risk may be up to 20-fold more prone to developing schizophrenia.”
The newfound genomic signals are not simply random sites of variation, say the researchers. They converge around pathways underlying the workings of processes involved in the disorder, such as communication between brain cells, learning and memory, cellular ion channels, immune function and a key medication target.
The Schizophrenia Working Group of the Psychiatric Genomic Consortium (PGC) report on their genome-wide analysis of nearly 37,000 cases and more than 113,000 controls in the journal Nature, July 21, 2014. The NIMH-supported PGC represents more than 500 investigators at more than 80 research institutions in 25 countries.
Prior to the new study, schizophrenia genome-wide studies had identified only about 30 common gene variants associated with the disorder. Sample sizes in these studies were individually too small to detect many of the subtle effects on risk exerted by such widely shared versions of genes. The PGC investigators sought to maximize statistical power by re-analyzing not just published results, but all available raw data, published and unpublished. Their findings of 108 illness-associated genomic locations were winnowed from an initial pool of about 9.5 million variants.
A comparison of the combined study data with findings in an independent sample of cases and controls yielded a high degree of replication, suggesting that considerably more such associations of this type are likely to be uncovered with larger sample sizes, say the researchers.
There was an association confirmed with variation in the gene that codes for a receptor for the brain chemical messenger dopamine, which is known to be the target for antipsychotic medications used to treat schizophrenia. Yet evidence from the study supports the view that most variants associated with schizophrenia appear to exert their effects via the turning on and off of genes rather than through coding for proteins.
The study found a notable overlap between protein-related functions of some linked common variants and rare variants associated with schizophrenia in other studies. These included genes involved in communication between neurons via the chemical messenger glutamate, learning and memory, and the machinery controlling the influx of calcium into cells.
“The overlap strongly suggests that common and rare variant studies are complementary rather than antagonistic, and that mechanistic studies driven by rare genetic variation will be informative for schizophrenia,” say the researchers.
Among the strongest associations detected, as in in previous genome-wide genetic studies, was for variation in tissues involved in immune system function. Although the significance of this connection for the illness process remains a mystery, epidemiologic evidence has long hinted at possible immune system involvement in schizophrenia.
Findings confirm that it’s possible to develop risk profile scores based on schizophrenia-associated variants that may be useful in research – but, for now, aren’t sensitive or specific enough to be used clinically as a predictive test, say the researchers.
They also note that the associated variations detected in the study may not themselves be the source of risk for schizophrenia. Rather, they may be signals indicating the presence of disease-causing variation nearby in a chromosomal region.
Researchers are following up with studies designed to pinpoint the specific sequences and genes that confer risk. The PGC is also typing genes in hundreds of thousands of people worldwide to enlarge the sample size, in hopes of detecting more genetic variation associated with mental disorders. Successful integration of data from several GWAS studies suggests that this approach would likely be transferrable to similar studies of other disorders, say the researchers.
“These results underscore that genetic programming affects the brain in tiny, incremental ways that can increase the risk for developing schizophrenia,” said Thomas Lehner, Ph.D., chief of NIMH’s Genomics Research Branch. “They also validate the strategy of examining both common and rare variation to understand this complex disorder.”
Reference
Biological insights from 108 schizophrenia-associated genetic loci. Schizophrenia Working Group of the Psychiatric Genomics Consortium. O’Donovan, et al. Nature. Online ahead of print 22 July 2014. doi:10.1038/nature13595.
Grants
MH094421
For more information: NIMH Director’s Blog, “Mapping the Risk Architecture of Mental Disorders”
About the National Institute of Mental Health (NIMH): The mission of the NIMH is to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery and cure. For more information, visit the NIMH website.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit the NIH website .
NIH…Turning Discovery Into Health®