Archived Content
The National Institute of Mental Health archives materials that are over 4 years old and no longer being updated. The content on this page is provided for historical reference purposes only and may not reflect current knowledge or information.
Brain’s Wiring Stunted, Lopsided in Childhood Onset Schizophrenia
Front-to-Back Wave Envelopes Brain as Child Grows Up
• Science Update
Growth of the brain's long distance connections, called white matter, is stunted and lopsided in children who develop psychosis before puberty, NIMH researchers have discovered. The yearly growth rate of this brain tissue was up to 2.2 percent slower-than-normal in such childhood onset schizophrenia (COS). The slower the rate, the worse the outcome — suggesting that this Magnetic Resonance Imaging (MRI) measure could someday lead to development of a biomarker that could aid treatment. Nitin Gogtay, M.D., and colleagues in the NIMH Child Psychiatry Branch and UCLA's Laboratory of Neuromaging report on their findings online in the Proceedings of the National Academy of Sciences during the week of October 13, 2008.
Background
Previous studies of COS by the NIMH/UCLA team had found a back-to-front wave of accelerated loss of the brain's working tissue — neurons and their immediate connections — called gray matter. White matter is so-named because these long-distance nerve fibers are protected by a white sheath of insulation. To measure white matter growth, the researchers scanned 12 children with COS and 12 healthy controls over five years. Superimposing one MRI scan onto another as they grew up grew up revealed how fast a child's white matter was growing in different brain areas. This was the first time this technique developed by UCLA's Paul Thompson, Ph.D., and colleagues, called tensor-based morphometry, had been used to study COS.
Results of This Study
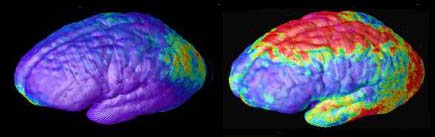
In contrast to gray matter, the wave of stunted white matter growth spread from front-to-back as the child grew up. The up to 2.2 percent slower than normal yearly growth rate was seen on the right side of the brain in COS. Even on the left side of the brain, the annual rate of white matter growth was only 1.3 percent in children with COS, compared 2.6 percent per year throughout the brain in controls. Children with COS who had higher white matter growth rates performed better on tests of brain function and had better prognoses.
Significance
Because the waves of net tissue reductions encroach from opposite directions, the findings put to rest earlier speculation that the gray matter loss might have resulted from white matter encroachment, say the researchers. Much like insulation makes an electrical wire more efficient, the white matter sheath on nerve fiber tracts normally thickens as we grow up, making for more efficient conduction of neural signals. The better functional outcomes in children with COS who had higher white matter growth rates may be attributable to this increased processing capacity, suggest the researchers.
What's Next?
The researchers cite as cause for hope the fact that the progressive deterioration in both gray and white matter is not yet complete at onset of psychosis in children with COS — perhaps leaving open "a window of opportunity" for future treatment interventions that might nip it in the bud. Imaging-based biomarkers of disease that could emerge from this line of studies hold promise for use in testing the efficacy of new treatments, said Gogtay. Tensor-based morphometry might also illuminate other neurodevelopmental conditions, such as certain forms of autism, in which white matter deficits have been implicated.
Childhood onset schizophrenia patients
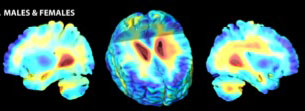
Healthy Controls
Average rates of white matter tissue growth (red) and tissue loss (blue) for healthy controls and childhood onset schizophrenia (COS) patients. COS patients' brains developed an asymmetrical pattern, with white matter growing at up to a 2.2 percent slower-than-normal yearly rate in the right hemisphere. 3-D tensor based morphometry MRI maps created from MRI scans of 12 patients and 12 matched controls over a 5-year period.
References
Gogtay N, Lu A, Leow AD, Klunder AD, Lee AD, Chavez A, Greenstein D, Giedd JN, Toga AW, Rapoport JL, Thompson PM. Three-dimensional brain growth abnormalities in childhood-onset schizophrenia visualized by using tensor-based morphometry. Proc Natl Acad Sci U S A. 2008 Oct 13. [Epub ahead of print] PMID: 18852461
Thompson PM, Vidal C, Giedd JN, Gochman P, Blumenthal J, Nicolson R, Toga AW, Rapoport JL. Mapping adolescent brain change reveals dynamic wave of accelerated gray matter loss in very early-onset schizophrenia. Proc Natl Acad Sci U S A. 2001 Sep 25;98(20):11650-5. PMID: 11573002
History
Text of NIMH News Update Posted November 8, 2001
Teens with Schizophrenia Lose Gray Matter in Back-to-Front Wave
Brains of teens with early onset schizophrenia are ravaged by a back-to-front wave of gray matter loss that parallels the progression from hallucinations and delusions to thinking and emotional deficits, National Institute of Mental Health (NIMH) — supported scientists have discovered. This loss of critical working brain tissue begins in rear perception processing areas, and over 5 years engulfs frontal areas responsible for functions like planning and reasoning. Although some loss of neurons and their branch-like extensions is normal during the teen years, as the brain prunes unused connections, the researchers had earlier shown that teens with childhood onset schizophrenia lose 4 times the normal amount in their frontal lobes. The new study is the first to visualize such a pattern of progressive tissue loss in schizophrenia. Paul Thompson, M.D., University of California, Los Angeles (UCLA), Judith Rapoport, M.D., NIMH, and colleagues, report on their findings in the September 25, 2001, Proceedings of the National Academy of Sciences.
Using magnetic resonance imaging (MRI), the researchers periodically scanned 12 teens with schizophrenia and 12 age-matched healthy teens over 5 years, beginning at age 14. The wave of gray matter loss began in an area above the ear and then spread forward. Since losses in the rear areas are thought to be caused by environmental factors, the findings are consistent with the notion that activation of some non-genetic trigger contributes to the onset and initial progression of the illness, suggest the researchers. The wave of loss correlated with worsening psychotic symptoms and mirrored the progression of neurological and cognitive deficits associated with the disorder. The final profile was consistent with the loss pattern in adult schizophrenia. Another group of 10 teens who were taking anti-psychotic medications for a different disorder did not show the same pattern of changes, reducing the likelihood that the gray matter losses were drug-induced.
The study is part of ongoing research on childhood onset schizophrenia by the NIMH Child Psychiatry Branch, which Rapoport heads. It employed a new 3-D MRI image analysis technique developed by NIMH grantee Arthur Toga, M.D, UCLA Laboratory of Neuroimaging, and colleagues. Support was also provided by grants from the NIH National Center for Research Resources, National Institute on Neurological Disorders and Stroke, and National Institute on Drug Abuse.
Also participating in the study were Jay Giedd, M.D., Peter Gochman, Jonathan Blumenthal, Robert Nicolson, M.D., NIMH, and Toga and Christine Vidal, UCLA.
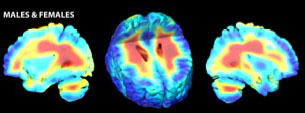
Areas of gray matter loss — shown in red and yellow — spread from back-to-front (right to left) over 5 years in composite MRI scan data from 12 teens with childhood onset schizophrenia, beginning at age 14 (left). Red and yellow denotes areas of greater loss.
Composite MRI scan data showing areas of gray matter loss over 5 years, comparing 12 normal teens (left) and 12 teens with childhood onset schizophrenia. Red and yellow denotes areas of greater loss. Front of brain is at left.
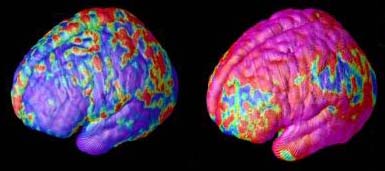
Time-Lapse MRI movie shows the brain developing in 12 teens with childhood onset schizophrenia. Areas of gray matter loss — red and yellow — spread from back-to-front over 5 years. These teens lost gray matter in the prefrontal cortex at 4 times the rate of normal health teens (see below).
Thompson PM, Vidal C, Giedd JN, Gochman P, Blumenthal J, Nicolson R, Toga AW, Rapoport JL. Mapping adolescent brain change reveals dynamic wave of accelerated gray matter loss in very early-onset schizophrenia. Proc Natl Acad Sci U S A. 2001 Sep 25;98(20):11650-5. PMID: 11573002.
MRI
Magnetic resonance imaging (MRI), provides a high resolution image of the brain's internal structure. The scanner contains a large magnet that induces different chemical elements to emit distinctive radio signals. The signal data is translated into 2-D pictures of the brain, slice by slice. These data can also be combined to create 3-D views (delete link it goes to old site). MRI is an important tool in studies of mental illnesses that may involve structural changes, such as schizophrenia and ADHD.